Mechanical Failure: Subsidence, Migration, and Stiffness Mismatch in Lumbar Fusion Cages
Cage Subsidence as a Primary Cause of Lumbar Fusion Cage Revision Surgery
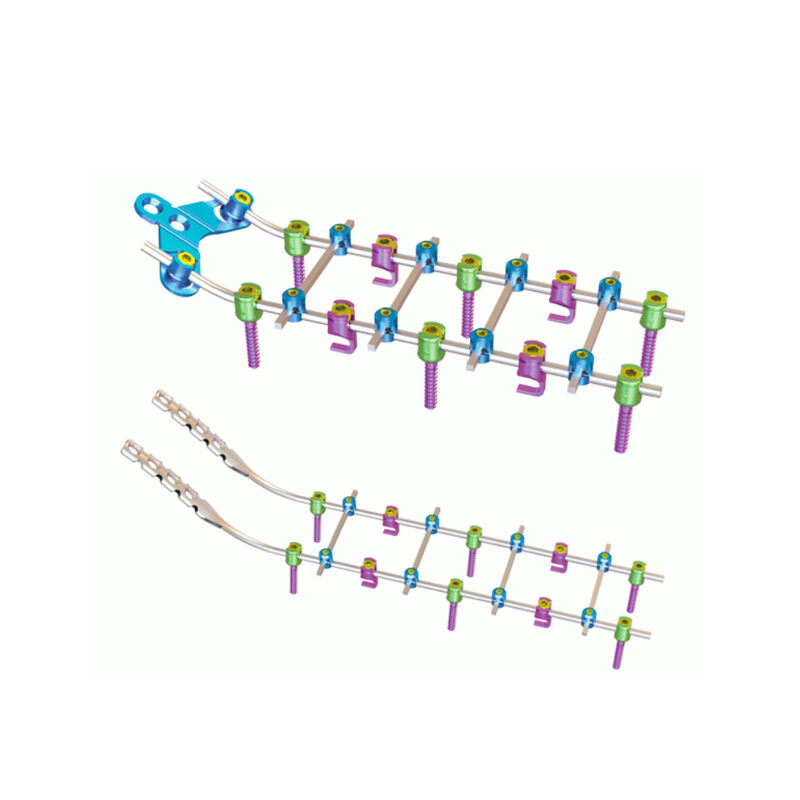
When implants sink into the vertebrae endplates, what we call cage subsidence happens in about 18 to 23 percent of cases where lumbar fusion cages need to be fixed or replaced. The main reasons behind this issue are weak bones, implants that are too big for the space, or when surgeons prepare the disc area too aggressively, which can damage the endplates themselves. As the disc gets shorter from subsidence, the openings where nerves exit get smaller, often leading back to those annoying nerve pains patients thought they were rid of. People with osteoporosis are especially at risk here, facing roughly three times more chance of problems compared to others, so checking bone strength before surgery really matters. Fixing these issues usually means taking out the old implant first, then filling up the vertebrae with special bone graft materials, and finally putting in new implants that have broader bases to spread out the pressure better across the spine.
Implant Migration and Its Contribution to Non-Union and Failed Back Syndrome
When implants migrate, especially when they move backward into the spinal canal or shift sideways toward important blood vessels, it really messes with the stability of the fusion bed. According to research published in the Spine Journal last year, this kind of movement accounts for about 31% of all non-union problems after surgery. The constant tiny movements stop bones from growing together properly in the space between vertebrae, which makes someone much more likely to develop failed back syndrome. Studies show patients with unstable implants face a 67% higher risk than those with good implant positioning. A few main reasons why this happens include using cages that are too small, not securing them properly, and mistakes made while placing them during surgery. For revisions, doctors typically add extra support from the back along with special growth factors like BMPs to help stabilize things mechanically and kickstart new bone formation.
Material Stiffness Mismatch: Disrupted Load Sharing and Pseudarthrosis Risk
Titanium cages, which have a stiffness around 110 GPa, actually push much more compressive force onto the surrounding endplates compared to PEEK options that range between 3-4 GPa. This creates what's called stress shielding, and it can really hurt the chances of successful bone grafts taking hold. When there's this big difference in stiffness, the normal way our bodies distribute loads gets messed up, so the fusion area doesn't get those important mechanical signals needed for proper bone growth. Biomechanical research shows that when implants are too stiff, the failure rate jumps all the way up to 15-30%. That's why smart design focuses on getting closer to the natural properties of trabecular bone, which sits somewhere between 10-20 GPa. Engineers achieve this balance using things like porous titanium structures or composite materials reinforced with carbon fibers. These approaches maintain necessary structural integrity while still allowing some flexibility, ultimately cutting down on the need for revisions later on.
Biological Failure: Inadequate Bone Healing and Graft-Related Lumbar Fusion Cage Revision Surgery Causes
Non-Union Due to Poor Osteoinduction, Graft Resorption, or Suboptimal Cage Design
When bones fail to grow across the space between vertebrae after surgery, this condition known as non-union becomes a major reason why doctors have to revise lumbar fusion cages. The problem usually happens because there isn't enough stimulation for bone growth, the graft gets absorbed too quickly, or sometimes just because the cage wasn't designed right for the patient's anatomy. While taking bone from another part of the body remains the best option for encouraging new bone growth, many surgeons avoid it due to risks at the donor site and limited amounts available. Synthetic alternatives simply don't contain those important proteins needed for proper healing, which explains why only about half of high-risk patients actually form new bone according to recent studies published in Spine Journal last year. When these graft materials break down too fast, especially if there's some movement issues or minor infections present, they create empty spaces that can shake loose the implant itself. Other problems include poor contact with the vertebral surfaces, mismatched rigidity causing stress points, and implants that are just too big for the area, all of which limit blood supply and make it harder for the graft to integrate properly. These factors together increase the chances of developing a false joint and ultimately lead to worse results when trying to fix non-unions through lumbar fusion procedures.
Revision Approaches for Pseudarthrosis: Cage Exchange vs. Structural Augmentation
Pseudarthrosis often needs another look when it comes to treatment, and the main aim here is getting back that mechanical stability along with proper biological function. When we talk about cage exchange, basically what happens is replacing that non-working implant with something bigger or better supported so the graft stays put and shares the load properly. This approach really shines for patients who have had serious subsidence issues or collapsed endplates. On the flip side, structural augmentation keeps the original cage intact but adds extra support from behind through instrumentation or BMPs, which helps boost fusion chances without tearing everything out again. The thing about revising cages though is they come with greater risk factors too, sometimes as high as one in four patients developing infections after surgery. But these revisions do provide better corrections when there's significant mechanical breakdown already present. Augmentation procedures tend to be gentler on the body overall, though doctors need to pick their candidates carefully, especially those dealing with osteoporosis or multiple level fusions. No matter which path gets chosen, tackling those hidden biological problems remains essential work. That means making sure the graft material works well, preparing those endplates just right during surgery, and fixing any metabolic issues such as low vitamin D levels or hyperparathyroidism if they exist, all of which play into whether healing sticks around long term.
Diagnostic and Clinical Errors Leading to Unnecessary or Ineffective Lumbar Fusion Cage Revision Surgery
Misdiagnosis Pitfalls: Distinguishing Pseudarthrosis from Adjacent Segment Disease or Radicular Pain
According to research published in The Spine Journal last year, incorrect diagnoses lead to roughly 15 to 20 percent of all unnecessary revision surgeries for lumbar fusion cages. Three conditions often confuse doctors: pseudarthrosis, adjacent segment disease (ASD), and radicular pain. These problems have similar symptoms but require completely different treatments. Pseudarthrosis usually causes pain that gets worse when moving around locally. ASD shows up as new nerve issues either above or below where the spine was fused. Radicular pain affects specific areas of skin following certain patterns that don't relate to how well the fusion held together. While CT scans and dynamic X-rays are still the go-to imaging methods, studies from the Journal of Neurosurgery show these tests leave about 30% of cases unclear. Relying too much on images alone without checking medical history, doing physical exams, and running nerve tests can easily point blame at the cage itself when it's not actually faulty. Choosing patients poorly for surgery matters too. People with untreated osteoporosis or ongoing spinal instability face even bigger chances of getting the wrong diagnosis. Getting this right matters because it helps prevent wasted procedures and leads to better results over time for those who need their fusions fixed properly.
FAQ
What causes cage subsidence in lumbar fusion surgeries?
Cage subsidence occurs when implants sink into the vertebrae endplates, often due to weak bones, oversized implants, or overly aggressive preparation of the disc area during surgery.
How does implant migration affect lumbar fusion surgery outcomes?
Implant migration destabilizes the fusion bed and can hinder bone growth between vertebrae, contributing to non-union issues and increasing the risk of failed back syndrome.
What is the impact of material stiffness mismatch on lumbar fusion cages?
A stiffness mismatch can lead to stress shielding, which disrupts normal load sharing and reduces the chance of successful bone grafting, increasing the risk of pseudarthrosis.
Why might a lumbar fusion cage revision be necessary?
Revisions are needed if there is non-union due to poor osteoinduction, graft resorption, suboptimal cage design, or significant mechanical and biological failures post-surgery.
How can misdiagnosis affect lumbar fusion surgeries?
Misdiagnoses can lead to unnecessary surgeries, as conditions like pseudarthrosis and adjacent segment disease can present with similar symptoms but require different treatments.
Table of Contents
- Mechanical Failure: Subsidence, Migration, and Stiffness Mismatch in Lumbar Fusion Cages
- Biological Failure: Inadequate Bone Healing and Graft-Related Lumbar Fusion Cage Revision Surgery Causes
- Diagnostic and Clinical Errors Leading to Unnecessary or Ineffective Lumbar Fusion Cage Revision Surgery
-
FAQ
- What causes cage subsidence in lumbar fusion surgeries?
- How does implant migration affect lumbar fusion surgery outcomes?
- What is the impact of material stiffness mismatch on lumbar fusion cages?
- Why might a lumbar fusion cage revision be necessary?
- How can misdiagnosis affect lumbar fusion surgeries?
 EN
EN
 FR
FR
 ES
ES
 AR
AR