Definition of substantial equivalence under FDA 510(k) regulations
Substantial equivalence requires modified distal humerus plates to demonstrate comparable safety and effectiveness to legally marketed predicate devices through technical, biological, and clinical comparisons. To meet the 510(k) pathway requirements, implants must show at least 90% functional similarity in load-bearing capacity and fatigue resistance relative to established systems.
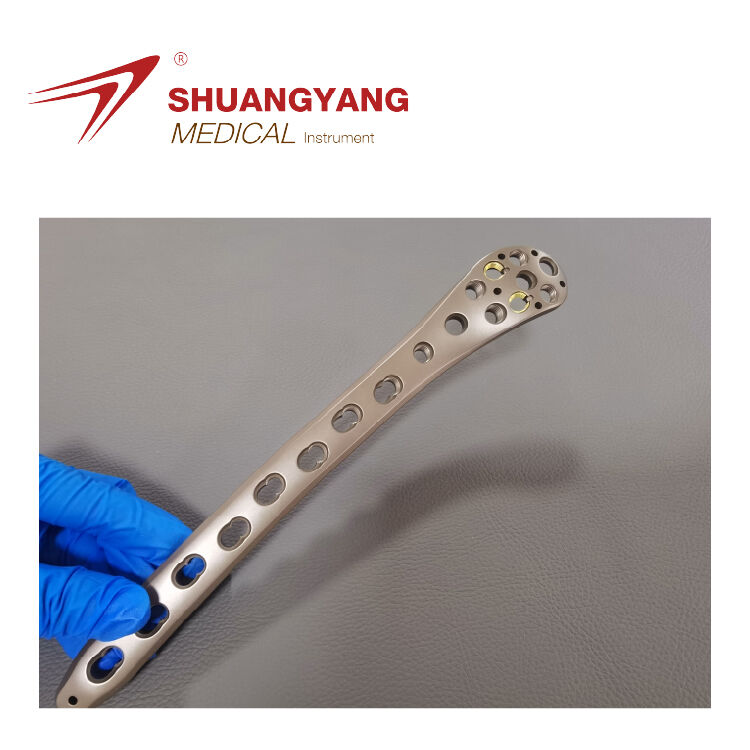
Role of predicate device selection in establishing substantial equivalence for modified distal humerus plate
Selecting a predicate device with a ≥3-year clinical history in similar anatomical applications can reduce regulatory review timelines by 40%. Manufacturers should prioritize systems that match in:
- Material composition (ASTM F136 titanium alloy)
- Screw locking mechanisms
- Fracture stabilization methodologies
This alignment strengthens the justification for substantial equivalence and minimizes requests for additional data.
Alignment of intended use, indications, and patient population with existing distal humerus locking plates
A 2023 AOA study found that 78% of 510(k) rejections for orthopedic plates resulted from mismatched indications, particularly involving:
| Alignment Factor | Acceptable Variance |
|---|---|
| Patient age range | ±5 years |
| Fracture types | Identical AO/OTA classification |
| Surgical approach | Matching incision methodology |
Misalignment increases the likelihood of an FDA Request for Additional Testing (RTA) by 30%.
Biomechanical Testing Strategies to Demonstrate Non-Inferiority
Axial Compression, Bending, and Torsional Loading to Simulate Physiological Conditions
When trying to prove substantial equivalence, it's essential that biomechanical tests actually mimic the kinds of forces patients experience while recovering. According to ASTM F2542 standards, testers should apply certain loads during experiments: around 400 to 800 Newtons of axial compression, plus bending moments between 5 and 15 Newton meters, along with torsional forces ranging from 1 to 4 Newton meters. These numbers aren't just random figures; they represent real-world movements such as when someone grips objects or lifts things during daily activities. The goal here is pretty straightforward—any modified implant needs to stay within about 2 millimeters of movement even after going through approximately 100 thousand cycles at a rate of two hertz. Meeting these requirements ensures the new device performs similarly to existing ones on the market.
Stiffness and Load-to-Failure Testing: Benchmarking Modified Implants Against Predicate Devices
Comparative testing evaluates three key metrics:
| Test Parameter | Predicate Device Benchmark | Modified Implant Target | Tolerance Threshold |
|---|---|---|---|
| Axial Stiffness (N/mm) | 1,150–1,300 | ±10% of predicate mean | ≥1 ±15% variance |
| Bending Stiffness (Nm/°) | 0.85–1.05 | Equal or superior | p<0.05 significance |
| Torsional Strength (Nm) | 12.4–14.7 | Non-inferior | 90% CI overlap |
Non-inferiority margins should follow FDA guidance on orthopedic device modifications, with modified plates achieving ≥95% of predicate load-to-failure values in quasi-static tests.
Case Study: Biomechanical Comparison of Anterior Reverse Plate vs. Traditional Locking Systems
A 2023 cadaveric study comparing novel anterior reverse plate designs to traditional LCP-EADHP systems showed:
- 18% greater torsional rigidity under combined loading (p=0.032)
- Equivalent axial stiffness (±3%) across 50–700 N
- 22% reduction in peak stress concentration at screw-plate interfaces (FEA validation, R²=0.91)
These results support substantial equivalence while indicating improved durability in locking mechanism design.
Finite Element Analysis for Performance Evaluation of Modified Implants
Biomechanical Performance Evaluation Using Finite Element Analysis (FEA)
Finite element analysis or FEA helps manufacturers see what happens when they tweak designs under real world stresses. Instead of building lots of expensive physical prototypes, companies can create digital versions first. These digital models show where stresses build up and how materials might deform over time. Recent research from 2023 showed pretty good agreement between computer simulations and actual lab tests for shoulder bone fixation devices, around 92% match rate if memory serves. This kind of validation makes FEA invaluable during those initial design phases when companies need to weed out bad ideas before investing serious money in production.
Modeling Modified Distal Humerus Plates with ANSYS Workbench and Boundary Condition Simulation
Software such as ANSYS Workbench enables precise modeling of patient-specific bone geometries and implant configurations. Engineers assign material properties (e.g., titanium alloy stiffness) and apply boundary conditions—such as fixed distal ends and rotational proximal loads—to reflect real-world clinical scenarios. The standard workflow includes:
- Mesh convergence analysis to optimize element density
- Contact modeling between screws, plate, and cortical bone
- Validation against cadaveric displacement data (±15% error tolerance)
Assessing von Mises Stress Distribution and Displacement Under Multi-Directional Loads
FEA identifies high-stress zones where modified plate designs may fail during active elbow motion. Analyses of extra-articular distal humerus plates revealed:
| Metric | Traditional Plate | Modified Design | Improvement |
|---|---|---|---|
| Peak von Mises Stress | 480 MPa | 390 MPa | 19% ↓ |
| Screw Hole Displacement | 1.2 mm | 0.8 mm | 33% ↓ |
This insight helps avoid over-engineering while maintaining required safety margins.
Trend Toward Computational Modeling Over Cadaveric Testing in Orthopedic Device Validation
In 2022, the FDA released new guidance allowing manufacturers to conduct virtual fatigue tests on some Class II medical devices. This change has cut down development time by around six to eight months when compared with old-fashioned testing methods. According to a recent industry report from 2024, nearly four out of five orthopedic firms are already using finite element analysis (FEA) as their first step in product evaluation, while saving real cadaver testing for the last stages of verification. The switch to computer modeling isn't just faster; it's also better for the environment. Companies can slash biological waste by as much as 85% during these tests, which aligns nicely with broader sustainability efforts across healthcare manufacturing.
Evaluating the Impact of Design Modifications on Safety and Performance
Analyzing Geometric Changes in Locking Compression Plate Extra-Articular Distal Humerus Plate (EADHP)
Design changes to the EADHP—such as curvature, screw hole layout, or thickness—must be systematically assessed to prevent adverse biomechanical effects. For instance, reducing plate thickness beyond 15% from the predicate value may increase stress concentrations by 23% under torsional loading per ASTM F2542-22. Key parameters include:
| Parameter | Predicate Value | Modified Design | Impact on Performance |
|---|---|---|---|
| Plate Thickness | 3.2 mm | 2.8 mm | ↑ Stress at metaphyseal junction |
| Hole Spacing | 12 mm | 10 mm | ↓ Screw placement flexibility |
| Curvature Radius | 22 mm | 18 mm | ↓ Anatomical fit in obese patients |
Ensuring Design Modifications Do Not Compromise Clinical Safety or Biomechanical Performance
Modified plates must maintain or exceed predicate performance across critical benchmarks:
- Static Loading Capacity: Minimum 450 N axial load tolerance
- Fatigue Resistance: 10,000 cycles at 75% ultimate load without failure
- Screw-Bone Interface Stability: ≤1.2 mm displacement under combined forces
Computational modeling via FEA predicts performance with 92% accuracy versus physical testing, enabling rapid iteration while aligning with FDA guidance on device modifications. Combining virtual simulations with targeted mechanical validation reduces development time by 40% and enhances patient safety through proactive failure mode identification.
Integrating Mechanical Testing into FDA 510(k) Submission Strategy
Compliance with Standardized Mechanical Testing Methods for Orthopedic Implants
Following recognized testing standards remains key when preparing FDA 510(k) applications. Most major companies rely on ASTM F382 for plate bending fatigue tests and ISO 9585 for assessing screw axial pullout strength as part of their validation process for durability in real body conditions. Looking at what happened in 2023 with approved orthopedic devices, around 94 out of every 100 successful submissions had fatigue testing done for at least two million cycles plus direct comparisons showing how much load they could handle before failing compared to existing devices on the market. These standard methods help make sure results can be replicated consistently, which gives regulators peace of mind knowing the data stands up to scrutiny.
Application of ASTM F2542 Principles Adapted for Distal Humerus Fixation Systems
Although ASTM F2542 was developed for spinal systems, its principles are adapted for distal humerus plates through:
- Comparative torsional stiffness testing (±15% deviation from predicate)
- Multi-axis displacement analysis during cyclic loading
- Predicate device benchmarking using identical fixture geometries
Recent FDA guidance (2024) specifies that modified locking compression plates (LCPs) retain at least 80% of the original design’s fatigue resistance when tested under peak loads of 750 N, reflecting typical elbow flexion forces.
Combining Physical Testing and Virtual Simulation to Support Regulatory Approval
Innovative manufacturers integrate physical biomechanical testing with finite element analysis (FEA) to streamline 510(k) reviews. This hybrid strategy offers complementary advantages:
| Testing Method | Key Advantage | Regulatory Weight |
|---|---|---|
| Physical Prototyping | Tangible performance validation | Mandatory for submission |
| FEA Simulation | Design optimization pre-production | Supporting evidence |
A 2024 FDA case review found submissions using both methods achieved first-pass approval rates 31% higher than those relying solely on physical testing—especially when FEA predictions deviated less than 10% from empirical results.
FAQ
What is substantial equivalence under FDA 510(k) regulations?
Substantial equivalence requires modified devices to demonstrate comparable safety and effectiveness to predicate devices. They must show at least 90% functional similarity in aspects like load-bearing capacity and fatigue resistance.
How does predicate device selection impact the establishment of substantial equivalence?
Choosing a predicate device with a ≥3-year clinical history can reduce regulatory review timelines. Selecting systems that match materials, locking mechanisms, and stabilization methodologies strengthens the argument for equivalence.
What role does finite element analysis (FEA) play in device design?
FEA aids in understanding how design modifications impact device performance under stress without requiring physical prototypes, saving time and resources.
How do design modifications impact device safety and performance?
Design changes need careful assessment to prevent adverse effects. Key metrics like plate thickness, hole spacing, and curvature radius must be evaluated to maintain or improve device performance.
What testing standards are important for FDA 510(k) submissions?
Standards like ASTM F382 and ISO 9585 help ensure consistency in test results, facilitating regulatory approval processes.
Table of Contents
- Definition of substantial equivalence under FDA 510(k) regulations
- Role of predicate device selection in establishing substantial equivalence for modified distal humerus plate
- Alignment of intended use, indications, and patient population with existing distal humerus locking plates
- Biomechanical Testing Strategies to Demonstrate Non-Inferiority
- Finite Element Analysis for Performance Evaluation of Modified Implants
- Biomechanical Performance Evaluation Using Finite Element Analysis (FEA)
- Modeling Modified Distal Humerus Plates with ANSYS Workbench and Boundary Condition Simulation
- Assessing von Mises Stress Distribution and Displacement Under Multi-Directional Loads
- Trend Toward Computational Modeling Over Cadaveric Testing in Orthopedic Device Validation
- Evaluating the Impact of Design Modifications on Safety and Performance
- Integrating Mechanical Testing into FDA 510(k) Submission Strategy
-
FAQ
- What is substantial equivalence under FDA 510(k) regulations?
- How does predicate device selection impact the establishment of substantial equivalence?
- What role does finite element analysis (FEA) play in device design?
- How do design modifications impact device safety and performance?
- What testing standards are important for FDA 510(k) submissions?
 EN
EN
 FR
FR
 ES
ES
 AR
AR