Understanding EU MDR Requirements and Reclassification of Maxillofacial Trauma Implants
Key Differences Between MDD and MDR Impacting Implant Classification
Moving from the old Medical Devices Directive to the new EU Medical Device Regulation has really stepped up the game when it comes to regulating maxillofacial trauma implants. Around 87 percent of what used to be classified as IIa or IIb devices are now considered higher risk according to Article 51(8) in the 2023 EU MDR framework. Manufacturers of these Class IIb implants face stricter rules now. They must deal with surprise factory inspections, provide better clinical data backing their products, and navigate new definitions around what counts as single-use equipment. These changes affect how hospitals handle reusable surgical tools too, since many instruments previously thought of as disposable might now fall under different regulations.
Reclassification of Maxillofacial Trauma Implants Under MDR: Implications for Audit Scope
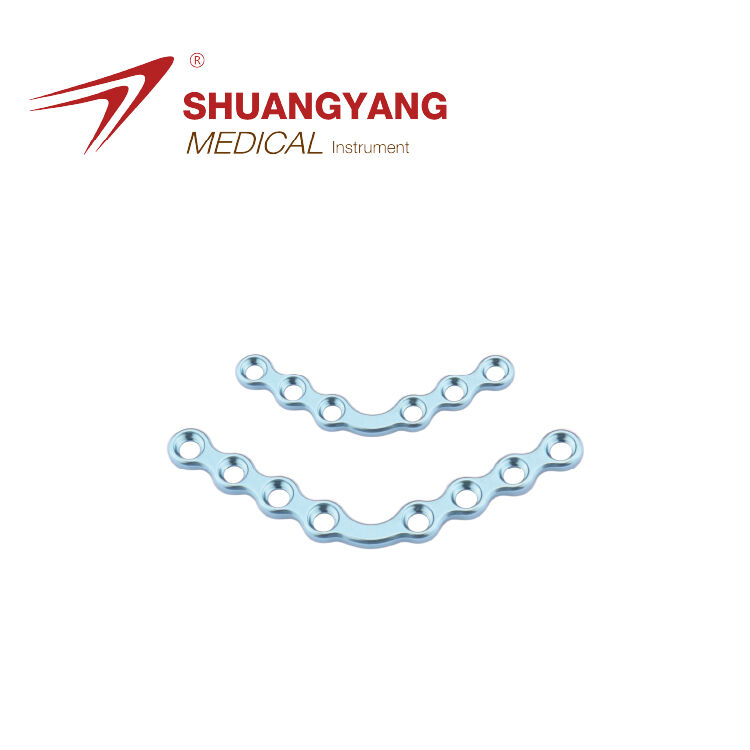
More than sixty percent of titanium mandibular plates along with zygomatic implants have been upgraded to Class IIb classification under the Medical Device Regulation (MDR). What does this mean? Well, manufacturers suddenly face three times the documentation requirements compared to what was needed under the old Medical Device Directive (MDD). The new rules also broaden the audit process significantly. Now companies must track materials all the way through production according to ISO 13485:2016 Clause 7.5.9 requirements. They need thorough validation of sterilization methods too. And there's an added layer about cybersecurity for those digital design files, something specifically mentioned in MDR Annex I Chapter II. These changes represent a major shift in compliance expectations for medical device makers working with these specific implant types.
General Safety and Performance Requirements (GSPR) in Annex I as Audit Benchmarks
The 23 General Safety and Performance Requirements (GSPRs) in MDR Annex I serve as primary audit benchmarks, demanding 40% more objective evidence than the former Essential Requirements under MDD. Key focus areas include:
| Audit Criterion | MDD Requirement | MDR Requirement |
|---|---|---|
| Biocompatibility | ISO 10993-1 | ISO 10993-18 (2023 update) |
| Mechanical Testing | 5-year data | 10-year aging validation |
| Clinical Benefit-Risk | Literature | Patient-specific outcomes |
Manufacturers must provide audit-ready documentation demonstrating a statistical correlation between implant surface roughness (Ra ≤ 3.2 μm) and long-term osseointegration success.
Conducting a Gap Analysis and Upgrading Technical Documentation per MDR Annex II
Successful MDR compliance for maxillofacial trauma implants begins with a structured gap analysis of legacy technical documentation. Research indicates 94% of manufacturers struggle to align design validation processes with Article 61 requirements, underscoring the need for systematic evaluation against MDR Annex II.
Assessing compliance gaps in legacy device documentation and design validation
Map existing technical files to MDR Annex II, focusing on whether design validation covers worst-case anatomical scenarios in facial trauma and includes 10+ year performance data from accelerated aging studies. Common deficiencies include incomplete material batch traceability and insufficient risk-benefit analyses for pediatric use.
Device description, materials, and surface properties for facial implants
Document titanium or PEEK alloy specifications with nanoscale surface topography measurements essential for osseointegration. For porous implants, quantify pore size distribution (100–500 μm) and strut thickness using micro-CT imaging per ISO 14630. Include SEM images confirming surface roughness below 5 μm to minimize soft tissue irritation.
Manufacturing processes and mechanical testing evidence for long-term performance
Ensure CNC machining parameters maintain <0.1 mm dimensional tolerance for custom mandible plates. Fatigue testing must simulate 10 million chewing cycles at 150N loads (ASTM F382), supported by finite element analysis correlating stress distribution with patient CT bone density data.
Biological evaluation and ISO 10993-compliant biocompatibility data
Update biological risk assessments using ISO 10993-1:2018 endpoints. Cytotoxicity testing must involve direct contact with 3D-printed implant surfaces. Surface characterization via XPS should confirm stable oxide layers, while justification for waiving carcinogenicity testing must be scientifically robust—addressing a key audit concern cited in industry reviews.
Developing a Robust Clinical Evaluation Report (CER) Under MDR Standards
Updating CERs per MEDDEV 2.7.1 Rev 4 with State-of-the-Art (SoTA) Review
A compliant CER must follow MEDDEV 2.7.1 Rev 4 and include a comprehensive State-of-the-Art (SoTA) review. This involves analyzing current scientific literature, competitor devices, and treatment alternatives to justify the safety and performance of maxillofacial implants. In 2023, 73% of EU manufacturers required urgent CER updates post-audit to meet GSPR requirements.
Demonstrating Equivalence with Predicate Devices Using Scientific Justification
The Medical Device Regulation (MDR) has made things tougher when it comes to proving equivalence between devices. Now manufacturers need to compare technical specs, biological properties, and clinical outcomes all at once. According to a recent Emergo Group report from 2024, nearly half (about 40%) of failed audits for Class IIb devices were due to poor material analysis or missing biomechanical test results. What works? Good equivalence submissions typically contain detailed finite element analyses showing how stress distributes across zygomatic implants, along with solid histological evidence about tissue compatibility. These combinations give regulators what they need to make informed decisions about device safety and effectiveness.
Leveraging Systematic Literature Reviews in Absence of Primary Clinical Trials
If primary clinical data isn't available, researchers should turn to PRISMA guided systematic reviews as an alternative approach. The process involves searching for relevant keywords that combine specific anatomical conditions like orbital floor fractures with different biomaterials such as PEEK or porous polyethylene. Researchers must apply strict inclusion and exclusion criteria according to EU MDR Annex XIV guidelines throughout their work. They also need to perform meta analyses based on at least five peer reviewed studies. These analyses help compare various complication rates including infection risks and implant extrusions. While this method takes time and effort, it remains one of the most reliable ways to gather meaningful insights when direct clinical evidence is lacking.
Common Pitfalls in MDR Clinical Evaluation Submissions for Class IIb Implantable Devices
Frequent audit findings include overreliance on pre-MDR literature without SoTA context, unjustified extrapolation of data from non-facial sites, and incomplete risk-benefit analyses comparing implant outcomes to autografts or other surgical alternatives.
Implementing Post-Market Surveillance and PMCF Plans for Ongoing Compliance
Designing PMS and PMCF Strategies for Class IIb and III Maxillofacial Implants
The EU Medical Device Regulation 2017/745 sets specific requirements for makers of Class IIb and III facial trauma implants regarding their post market surveillance activities. According to Annex III guidelines, these companies need to develop appropriate PMS plans that match the level of risk associated with their products. When it comes specifically to titanium mesh used in craniofacial applications, there are several key areas they should focus on. Monitoring how well these implants hold up mechanically in actual clinical settings is critical. We're talking about things like fracture rates when patients chew food normally. Another important aspect involves keeping tabs on infection rates after surgery, particularly looking at how different surface treatments affect outcomes. Plasma spray coatings come up frequently here. Manufacturers also have to remember to review and adjust their PMCF strategies every year as new data becomes available from ongoing studies and clinical experiences across Europe.
Integrating Real-World Clinical Feedback into Safety and Performance Monitoring
According to TÜV SÜD's 2023 audit findings, about 62 percent of problems under the Medical Device Regulation come down to how companies handle data after products hit the market. Smart manufacturers are tackling this issue head on through various approaches. Many have started setting up automated systems that look at complications reported by surgeons like when implants move out of place in the cheek area. They also check customer complaints against what labs find when they examine returned devices. Some companies even use advanced analytics tools to spot potential compliance issues before they become major headaches.
Linking Post-Market Data to Periodic Safety Update Reports (PSURs)
Annual PSURs must include:
| Data Category | Required Metrics for Maxillofacial Implants | MDR Reference |
|---|---|---|
| Clinical | Reoperation rates linked to material fatigue (ISO 14602) | Annex III.1a |
| Technical | Sterilization batch failures affecting porous titanium structures | Annex II.6.2 |
| Regulatory | CAPA timelines for adverse event resolution | Article 88(3) |
This integrated lifecycle approach reduces audit findings by 41% compared to legacy MDD programs, according to the BSI Medical Devices Report 2024.
Achieving Notified Body Readiness: QMS Alignment and Mock Audits
Successful MDR audit preparation requires full alignment of quality systems with regulatory expectations. Manufacturers must demonstrate end-to-end traceability and proactive risk management to satisfy Notified Body requirements under the EU's stringent framework.
Aligning Quality Management System with MDR Article 10 and ISO 14971 Risk Management
Integrate MDR Article 10 obligations into your QMS by aligning design controls, supplier management, and post-market surveillance with ISO 14971 risk principles. Audit trends show 68% of non-conformities relate to weak risk-benefit documentation for implants. Establish cross-functional teams to review biocompatibility, sterilization, and mechanical testing within an MDR-compliant risk framework.
Conducting Internal Mock Audits and Preparing for Unannounced Assessments
Conduct quarterly mock audits simulating Notified Body evaluations, focusing on gaps in material traceability and clinical evidence. Prepare for unannounced inspections by validating UDI implementation across batches, verifying electronic QMS audit trails, and training staff on real-time retrieval of device history records.
Ensuring Traceability from Design Inputs to Clinical Claims During Audits
Creating a two-way traceability system that connects material specs, mechanical properties, and actual patient results makes good sense for all types of implants. The numbers tell a story too many companies overlook - about 4 out of 10 manufacturers struggle to link those customer complaints after product release back to their original design tests. Automated software can help bridge this gap by showing exactly how lab-based fatigue tests on titanium mesh implants match up against what doctors actually report in periodic safety update reports. While no tool is perfect, these digital solutions offer a practical way forward when trying to close the loop between theoretical performance and real world experience.
FAQ Section
What are the significant changes in implant classification due to the transition from MDD to MDR?
The transition has led to about 87% of previously classified IIa or IIb devices now being considered higher risk, resulting in stricter regulations and added responsibilities for manufacturers.
What are the implications of reclassification for the audit scope under MDR?
More than sixty percent of certain implants have been upgraded to Class IIb, leading manufacturers to face three times the documentation requirements and expanded audit processes.
Why is conducting a gap analysis important for MDR compliance?
Conducting a gap analysis helps manufacturers systematically evaluate existing documentation against new MDR standards, ensuring compliance and addressing any deficiencies.
What strategies can manufacturers use for successful MDR audits?
Strategies include aligning QMS with MDR Article 10 and ISO 14971, conducting internal mock audits, and ensuring traceability from design inputs to clinical claims.
Table of Contents
- Understanding EU MDR Requirements and Reclassification of Maxillofacial Trauma Implants
-
Conducting a Gap Analysis and Upgrading Technical Documentation per MDR Annex II
- Assessing compliance gaps in legacy device documentation and design validation
- Device description, materials, and surface properties for facial implants
- Manufacturing processes and mechanical testing evidence for long-term performance
- Biological evaluation and ISO 10993-compliant biocompatibility data
-
Developing a Robust Clinical Evaluation Report (CER) Under MDR Standards
- Updating CERs per MEDDEV 2.7.1 Rev 4 with State-of-the-Art (SoTA) Review
- Demonstrating Equivalence with Predicate Devices Using Scientific Justification
- Leveraging Systematic Literature Reviews in Absence of Primary Clinical Trials
- Common Pitfalls in MDR Clinical Evaluation Submissions for Class IIb Implantable Devices
- Implementing Post-Market Surveillance and PMCF Plans for Ongoing Compliance
- Achieving Notified Body Readiness: QMS Alignment and Mock Audits
-
FAQ Section
- What are the significant changes in implant classification due to the transition from MDD to MDR?
- What are the implications of reclassification for the audit scope under MDR?
- Why is conducting a gap analysis important for MDR compliance?
- What strategies can manufacturers use for successful MDR audits?
 EN
EN
 FR
FR
 ES
ES
 AR
AR