Understanding UDI and Its Importance for Locking Screw Orthopedics
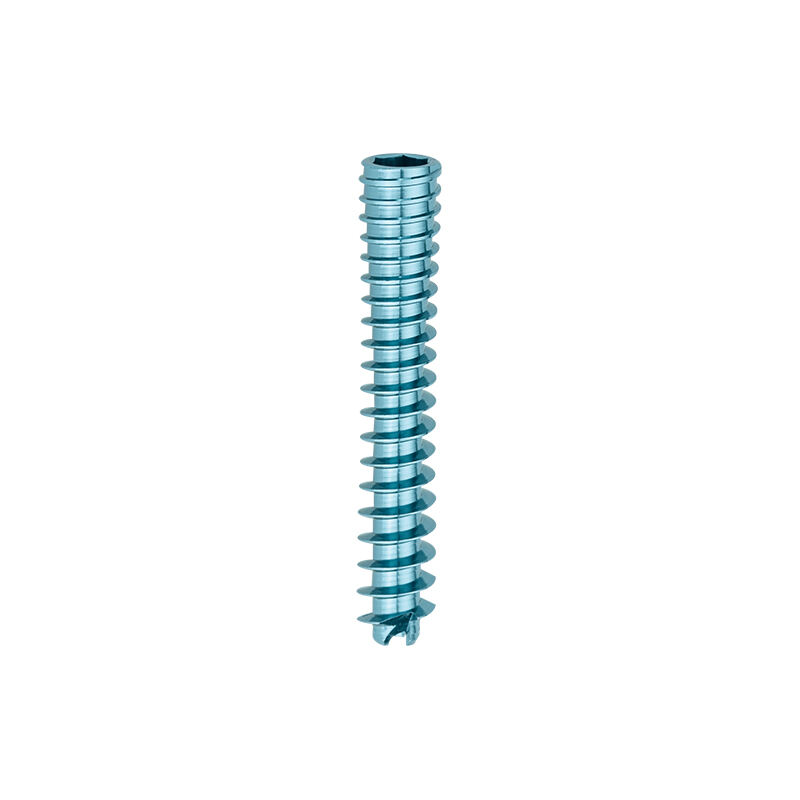
What makes UDIs so important for orthopedic implants? Let's take locking screws as an example these are the ones that hold broken bones together during healing. According to recent FDA data, around one out of every six medical device recalls from 2020 through 2023 had something to do with being unable to track where implantable devices came from. When hospitals give each screw a standardized UDI code that can be scanned, they get immediate access to information about who made it, what batch it was produced in, and when it expires. The benefits are pretty clear. Surgical mistakes drop significantly, and when problems arise, hospitals respond to recalls much faster than before. Some studies show this improvement cuts down response times by nearly two thirds compared to old fashioned paper records. That matters a lot when patient safety is at stake.
Core Components of UDI: Device Identifier (DI) and Production Identifier (PI)
Every UDI contains two key elements:
- Device Identifier (DI): A fixed, alphanumeric code specific to the device model (e.g., “LXS-45” for a 4.5mm titanium locking screw).
- Production Identifier (PI): Variable details like production date (“2025-01”), batch number (“BATCH227”), and sterilization expiry (“2026-06”).
These components enable precise lifecycle tracking—from factory to implantation—and align with ISO 13485 quality management standards.
There's good reason why locking screws need those implant level UDI labels on them. These little guys actually carry weight in fixing fractures, so tracking them matters quite a bit. According to regulations from the EU Medical Device Regulation, any screw under 8 millimeters must have what they call direct part marking. This ensures that even after surgery when everything gets put together, doctors can still read those important numbers. Some research came out last year showing that these marked screws cut down mistakes during operations where multiple parts are involved, especially in tricky spinal procedures. Around eighty one percent fewer errors? That sounds pretty impressive. And beyond just helping surgeons, having this detailed information at the implant level makes it possible to track problems if something goes wrong later on. When issues pop up with certain devices, manufacturers can pinpoint exactly which batch might be causing trouble.
FDA UDI Rules for Orthopedic Screws and Surgical Implants
Under regulations found in 21 CFR 801.20, the FDA requires orthopedic locking screws to meet UDI standards. This means manufacturers must put both the Device Identifier (DI) and Production Identifier (PI) right on product labels and packaging materials. For Class II medical devices like spinal screws and various trauma fixation systems, there's an additional requirement: expiration dates along with batch numbers need to appear in formats that people can read easily as well as through automated identification systems. Looking at recent trends since mid-2022 shows just how critical proper labeling really is. Nearly all implant recalls during this period were linked somehow to incomplete or missing UDI information according to reports from the FDA released last year. Because of this problem, companies are increasingly focused on submitting comprehensive details about their products into the GUDID database. Important specifications such as physical dimensions, how devices get sterilized, and whether they work safely with MRI machines have become standard requirements for submission these days.
EU MDR UDI Mandates and Their Impact on Locking Screw Devices
The EU MDR Annex VI requires orthopedic screw manufacturers to register their Basic UDI-DI information in EUDAMED prior to bringing products to market. This differs from FDA requirements where such detailed tracking isn't mandated at the same level. European regulations actually go further than many expect, requiring UDI markings at the individual implant level for both single use and reusable devices. And these aren't just any markings either they must be verified as compliant with ISO 13485 standards when using laser etching techniques. According to a recent industry survey published by NBOG in 2023, nearly half (around 42%) of manufacturers operating within the EU encountered compliance issues last year because their technical documentation failed to properly connect UDI data with necessary clinical evaluation records.
Key Differences Between FDA and EU MDR UDI Standards
| Criteria | FDA UDI Requirements | EU MDR UDI Requirements |
|---|---|---|
| Database Submission | GUDID (device attributes only) | EUDAMED (technical + clinical data) |
| Unique Identifier Scope | Commercial packaging and device labels | Device itself (implant-level marking) |
| Timelines | 6-24 months post-classification | 12 months before clinical use |
FDA prioritizes post-market surveillance, while EU MDR integrates UDI with PMS obligations and stricter notified body oversight.
UDI Labeling and Marking Challenges for Small Orthopedic Screws
Implementing UDI on locking screws presents unique hurdles due to their miniature size and strict regulatory demands. A 2023 medical device labeling study found 42% of manufacturers struggle with achieving permanent legibility on implants smaller than 5mm, risking non-compliance with FDA and EU MDR traceability rules.
Direct Part Marking (DPM) Techniques for Locking Screws
DPM methods must balance durability with minimal material impact:
- Laser etching: Preferred for stainless steel/titanium screws, achieving 0.2mm character heights (meets FDA 21 CFR Part 830 requirements)
- Electrochemical marking: Suitable for cobalt-chrome alloys, with 99.9% post-sterilization readability in validation tests
- Micro-engraving: Used when surface oxidation risks exist, though it adds 15-20 seconds per unit to production time
Compliance with UDI Carrier Standards (GS1, HIBCC) on Miniature Devices
Adhering to GS1's 1.5mm minimum barcode height requires innovative approaches:
- Reduced symbology: Data Matrix codes at 0.3mm x 0.3mm size (ISO/IEC 16022 compliant)
- Multi-layer marking: Combining laser-etched text with surface-applied QR codes (72% success rate in recent pilot programs)
- Automated verification systems: Machine vision tools that validate markings at 50x magnification during packaging
Manufacturers achieving <0.5% UDI rejection rates typically integrate robotic handling with real-time laser calibration, ensuring consistent marking quality across batch sizes from 100 to 100,000 units.
GUDID Submission and Data Management for Locking Screw Devices
Step-by-Step Process for Submitting UDI Data to GUDID
To comply with FDA UDI requirements, orthopedic manufacturers must submit detailed locking screw data to the Global Unique Device Identification Database (GUDID). The process involves:
- Data Collection: Gather DI (Device Identifier) and PI (Production Identifier) information, including lot numbers, expiration dates, and sterilized-by dates.
- Formatting: Adhere to FDA’s HL7 SPL standards for XML-based submissions.
- Validation: Use the FDA’s GUDID Web Interface to verify formatting compliance before final submission.
A 2023 FDA audit revealed that 97% of orthopedic implant rejections stem from incorrect production date formatting or missing sterilization data. Manufacturers targeting EU markets should cross-reference EUDAMED submissions with GUDID entries to avoid regulatory mismatches.
| Key GUDID Data Fields for Locking Screws | Format Requirements |
|---|---|
| Device Identifier (DI) | GS1 GTIN-14 or HIBCC LHIC |
| Production Identifier (PI) | ISO 8601 date format (YYYY-MM-DD) |
| Implant Dimensions | Millimeters (e.g., 3.5mm x 22mm) |
Leveraging Automation for Accurate and Efficient UDI Documentation
Leading manufacturers reduce manual errors by implementing automation tools for UDI documentation. Cloud-based systems with integrated FDA/EU MDR validation rules can:
- Auto-generate GS1-compliant barcodes for screws <4mm in diameter
- Flag discrepancies between PI data and manufacturing records
- Synchronize updates across GUDID and internal ERP systems
A 2023 study showed automated UDI workflows reduced documentation errors by 40% in locking screw production compared to manual methods. Real-time validation APIs now enable instant feedback on data formatting, critical for maintaining compliance as FDA expands UDI requirements to Class II devices.
Frequently Asked Questions
What is a UDI and why is it important for orthopedic implants?
A UDI, or Unique Device Identifier, is a standardized code used to identify medical devices like orthopedic implants. It's crucial because it helps in tracking the device's origin, manufacturer, batch, and expiration date, significantly reducing surgical mistakes and speeding up recall responses.
What are the main components of a UDI?
A UDI consists of two main elements: the Device Identifier (DI) and the Production Identifier (PI). The DI is a fixed alphanumeric code specific to the device model, while the PI includes variable details like production date, batch number, and sterilization expiry.
How do FDA and EU MDR UDI requirements differ?
The FDA's requirements focus on submitting device attributes to the GUDID database, while the EU MDR mandates registration of technical and clinical data in EUDAMED. The EU MDR requires UDI markings at the individual implant level, whereas the FDA focuses on commercial packaging and device labels.
What challenges do manufacturers face in implementing UDI on small orthopedic screws?
Manufacturers encounter challenges like ensuring permanent legibility on tiny implants, meeting regulatory standards, and employing direct part marking techniques that balance durability without significantly impacting material.
How does automation help in maintaining UDI compliance?
Automation tools help reduce manual errors by synchronizing updates across databases, auto-generating compliant barcodes, and flagging discrepancies between PI data and manufacturing records, ultimately enhancing accuracy and efficiency.
Table of Contents
- Understanding UDI and Its Importance for Locking Screw Orthopedics
- FDA UDI Rules for Orthopedic Screws and Surgical Implants
- EU MDR UDI Mandates and Their Impact on Locking Screw Devices
- Key Differences Between FDA and EU MDR UDI Standards
- UDI Labeling and Marking Challenges for Small Orthopedic Screws
- GUDID Submission and Data Management for Locking Screw Devices
- Frequently Asked Questions
 EN
EN
 FR
FR
 ES
ES
 AR
AR