From Traditional Implants to Additive Manufacturing in Craniofacial Surgery
Limitations of Conventional Premolded Titanium Mesh in Complex Facial Reconstructions
Traditional titanium mesh implants that come pre-molded just don't cut it when dealing with the complicated shapes found in craniofacial defects. The problem is these standard designs can't really match up with those tricky areas like orbital floors, zygomatic arches, and frontal sinuses either. According to JAMA Surgery from last year, about 38% of patients end up with implants that don't fit properly. What happens next? Surgeons find themselves spending anywhere between twenty to forty minutes during surgery trying to bend these pre-formed meshes into shape. This extra work isn't just time consuming though it actually puts the material at risk of breaking down over time and raises chances of infection too. And all this leads to pretty significant problems down the road. We're seeing revision surgery rates hit around 15% for those complicated midface reconstruction jobs, especially after accidents or birth defects create asymmetry issues.
The Shift to Patient-Specific Implants Enabled by Additive Manufacturing
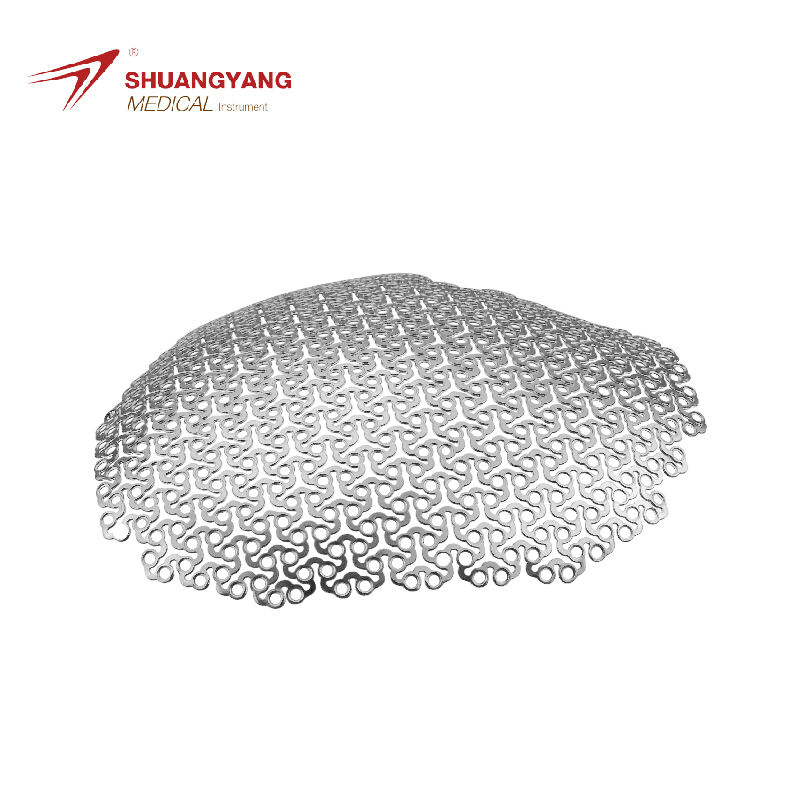
The field of craniofacial reconstruction has changed dramatically thanks to additive manufacturing technology and its ability to create custom titanium meshes for individual patients. When doctors take CT scans of a patient's skull and feed that information into 3D printers, they can produce implants that match the original bone structures down to fractions of a millimeter. According to recent research published in the Journal of Cranio-Maxillofacial Surgery last year, this level of precision helps restore proper facial symmetry in almost all cases, with success rates around 96%. What makes this approach so groundbreaking is how it replaces old manual techniques with a completely digital process. Surgeons no longer need to shape metal by hand because these printed implants already have built-in porosity patterns that closely resemble actual bone density variations. Many top medical centers are now combining this technology with advanced navigation tools during surgery, allowing them to place implants exactly where needed without guesswork.
How 3D Printing Is Transforming Surgical Planning and Implant Design
The field of preoperative planning has really taken off since additive manufacturing started working hand in hand with surgical simulation tools. Today's surgeons get to play around with virtual implants on actual patient anatomy models made in 3D. They can tweak where screws go to steer clear of blood vessels and create strong but lightweight mesh parts using those fancy lattice designs that cut down weight by about 40%. What does this mean in practice? For operations involving the orbital floor, surgery times have dropped quite a bit—from roughly 3 hours and 12 minutes down to just under two hours when using these AM techniques. Plus there are fewer problems after surgery too, which makes everyone involved pretty happy.
Precision and Customization: Achieving Anatomical Accuracy with 3D-Printed Titanium Mesh
The field of craniofacial reconstruction has seen major improvements in anatomical accuracy thanks to additive manufacturing techniques, especially when dealing with complicated situations where titanium mesh implants are needed. Traditional premolded options basically follow a one size fits all approach, but 3D printed titanium mesh works differently. It uses specific patient data to create replicas that match the natural curves and varying thicknesses of bones down to about half a millimeter accuracy. What this means is surgeons don't have to bend things as much during surgery, which makes everything more stable over time. The way these implants distribute pressure matters a lot too, particularly in parts of the face that need to support weight such as around the eye socket area.
Digital Workflow from CT Scan to Patient-Matched Titanium Mesh Design
It all starts with those detailed CT scans getting transformed into 3D models through special segmentation software. Doctors work hand in hand with engineers to create custom mesh designs that fit exactly where there are bone defects in patients. They have to be careful around nerves and blood vessels while also making sure everything looks symmetrical when put back together. Some research from last year showed pretty impressive results too. The new method cut down on how long surgeons spend planning operations by almost a third compared to old fashioned manual tracing techniques which took forever.
Enhancing Facial Symmetry and Implant Fit Through Additive Manufacturing
With 3D printing, we can make really fine adjustments to how porous the mesh is (around 45 to 85 percent customizable) and create different thicknesses that actually look like real bone structures next to them. A recent study looked at 112 cases where people needed cheekbone reconstruction. Those who got 3D printed implants ended up with much better symmetry after surgery - about 92 percent compared to just 68 percent for traditional mesh implants. The big reason? This new tech just does a far better job at copying those tiny details in the jaw angle and around the eye socket area that are so important for natural appearance.
Case Study: Efficient Orbital Floor Reconstruction Using Pre-Fabricated 3D-Printed Mesh
A small study involving just 14 patients who needed repairs to their orbital floors demonstrated how effective 3D printing can be in surgery. Using images taken before surgery, doctors created custom mesh implants for each person, complete with built-in channels for screws that matched up perfectly with what remained of their bone structure. Because these implants were already shaped exactly right, there was no need to adjust them during actual operations. The results were pretty impressive too. Surgery times dropped dramatically from an average of over two hours down to barely an hour, and the accuracy of where the implants ended up improved by almost four out of five cases compared to traditional methods.
Reducing Intraoperative Adjustments and Surgical Time with Custom Solutions
Eliminating manual mesh bending correlates directly with shorter anesthesia exposure and lower infection risks. Data from 86 maxillofacial reconstructions shows 3D-printed custom solutions decreased operating room time by 41% compared to traditional methods. Surgeons report 64% fewer instrument passes during implantation due to pre-optimized screw hole alignment and edge geometry.
Engineering Biomimetic, Porous Titanium Mesh via Additive Manufacturing
Using additive manufacturing techniques allows engineers to create titanium mesh with pores sized between 200 and 500 micrometers, similar to how natural bone tissue is structured. These specific pore dimensions strike a balance between structural integrity and biological function, as they provide channels for blood vessels to grow through while still allowing bone cells to move into the implant area. Research published last year showed some interesting results too. Implants featuring around 350 micrometer pores had nearly double the success rate when it came to attaching osteoblasts, at 89 percent versus just 52 percent for older solid mesh designs that don't have these specialized pores built in.
| Pore Size (Լm) | Bone Ingrowth Rate (%) | Vascularization Density (vessels/mm²) |
|---|---|---|
| 200 | 74 | 18 |
| 350 | 89 | 34 |
| 500 | 67 | 26 |
Selective laser melting (SLM) allows gradient porosity designs, where dense regions support load-bearing facial areas and porous zones enhance biological integration. Researchers now use triply periodic minimal surface (TPMS) algorithms to generate self-supporting lattice architectures, reducing material waste by 22% without compromising strength.
Improved Bone and Soft Tissue Integration in 3D-Printed Craniofacial Implants
Porous titanium made through 3D printing integrates with bone tissues about 78 percent faster compared to traditional premolded mesh options. This happens because the interconnected pore structure allows nutrients to flow better while making it easier for bone cells to settle in and grow. When we modify these surfaces using techniques like plasma electrolytic oxidation, we get surfaces that attract water and have tiny textures at the nano level. These changes boost protein sticking to the surface roughly three times more than standard materials, which definitely speeds up new bone growth. Looking at real world results, clinical tests found that around 94% of facial implants featuring those special microgrooves between 25 and 50 micrometers wide managed full soft tissue integration within just eight weeks. This not only helps tissues heal properly but also cuts down chances of infections happening later on. Research published in 2024 examined 412 cases where doctors rebuilt eye sockets and found something pretty impressive: when they used custom printed mesh instead of off-the-shelf products, patients needed far fewer follow-up surgeries over five years time period. The number dropped from nearly 19% needing corrections down to just 4%, all because the printed parts fit the body's natural shape so much better.
Clinical Benefits and Economic Considerations of 3D-Printed Titanium Mesh
Evidence-Based Outcomes: Shorter Hospital Stays and Reduced Revision Surgeries
The use of additive manufacturing has made it possible to create titanium mesh implants specifically matched to individual patients, cutting down on post surgery problems by around 43% compared to those old fashioned premolded options according to research published in the Journal of Craniofacial Surgery back in 2023. When doctors work with these custom 3D printed parts, they no longer need to bend them during surgery something that causes about 22% of all delays in fixing broken orbital floors. Many surgeons have noticed their procedures take about 32% less time overall when working with these pre made implants that fit within just under 1 mm of the actual anatomy. All these improvements mean real differences in how well patients recover after their operations.
- 1.9-day average reduction in hospitalization for complex maxillofacial reconstructions
- 67% lower revision surgery rates at 12-month follow-ups
- 89% patient satisfaction with aesthetic outcomes versus 54% for standard mesh
Balancing Cost-Effectiveness and Accessibility of Additive Manufacturing in Healthcare
The initial cost of producing 3D printed titanium mesh implants does come in at around 28% more expensive compared to standard options available off the shelf. However, hospitals end up saving money overall thanks to several factors. They see about 19% in total savings when looking at things like less wasted sterile inventory, fewer repeat operations needed, and shorter times spent in surgery rooms. When manufacturers produce parts just when they're needed, inventory waste drops by roughly 40%. And for every individual case handled this way, hospitals save approximately $8,500 simply because there's no need for corrective procedures later on. Plus, surgical teams spend about 15% less time in the operating room, which obviously brings down expenses across the board. The insurance landscape is changing too. Seven different states across America have started covering between 80 to even 100% of the costs associated with additive manufacturing specifically for facial bone reconstructions since early 2024. This shift represents a major step forward for both medical facilities and patients alike.
Overcoming Barriers to Adoption: Regulatory and Scalability Challenges
In 2023, the FDA introduced a new fast track for approving custom cranial implants, slashing what used to take about 14 months down to just under three months now. But there's a catch. Only around one third of American hospitals actually have the proper certifications needed to run their own 3D printing operations according to ISO standards. So how are companies trying to scale this technology? Well, they're investing heavily in automated design tools that can knock weeks off the development process. Some firms report cutting design time by nearly four fifths with these systems. At the same time, manufacturers are rolling out industrial grade printers equipped with multiple lasers that speed up titanium mesh fabrication by almost half. And we're starting to see regional printing centers pop up across the country, each typically handling between five and seven different hospital orders at once.
FAQ
What are the main advantages of using 3D-printed titanium mesh in craniofacial surgery?
The main advantages include achieving customized fit and anatomical accuracy, reducing intraoperative time and manual adjustments, enhancing bone and soft tissue integration, and decreasing the risk of post-surgery complications.
How does 3D printing improve surgical outcomes in facial reconstructions?
3D printing allows for the creation of patient-specific implants that fit accurately, reducing surgical time and lowering the risk of complications. It improves aesthetic results and speeds up recovery by facilitating better integration with bone and soft tissue.
Are there economic benefits to using 3D-printed implants in surgery?
Yes, while the initial production costs may be higher, overall savings are achieved through reduced surgery times, less waste in sterile inventory, decreased need for revision surgeries, and shorter hospital stays.
What are the challenges to wider adoption of 3D-printed implants in medical facilities?
Challenges include the need for facilities to obtain proper certifications for running 3D printing operations, regulatory approvals, scalability of production, and initial infrastructure investment.
Table of Contents
- From Traditional Implants to Additive Manufacturing in Craniofacial Surgery
-
Precision and Customization: Achieving Anatomical Accuracy with 3D-Printed Titanium Mesh
- Digital Workflow from CT Scan to Patient-Matched Titanium Mesh Design
- Enhancing Facial Symmetry and Implant Fit Through Additive Manufacturing
- Case Study: Efficient Orbital Floor Reconstruction Using Pre-Fabricated 3D-Printed Mesh
- Reducing Intraoperative Adjustments and Surgical Time with Custom Solutions
- Engineering Biomimetic, Porous Titanium Mesh via Additive Manufacturing
- Improved Bone and Soft Tissue Integration in 3D-Printed Craniofacial Implants
- Clinical Benefits and Economic Considerations of 3D-Printed Titanium Mesh
 EN
EN
 FR
FR
 ES
ES
 AR
AR