MRI Safety Fundamentals for Anterior Cervical Spine Implants
Decoding ASTM F2503: Magnetic Resonance Conditional, Safe, and Unsafe Classifications
When it comes to MRI safety for anterior cervical spine implants, everything starts with the ASTM F2503 standard. This is basically the go-to system worldwide for categorizing medical devices into three main groups: MR Safe, MR Conditional, and MR Unsafe. The standard looks at what happens to implants during MRI scans, focusing specifically on things like torque forces, heat buildup, and image artifacts. These assessments form the basis for proper patient screening before any scan takes place. Devices labeled MR Safe, such as those made from non-metallic polymers, generally don't present any problems regardless of MRI conditions. Most titanium implants fall into the MR Conditional category though. These are considered safe only if certain parameters are met, like keeping the magnetic field strength below 1.5 Tesla and staying within specific gradient limits. Then there are the truly dangerous ones marked MR Unsafe, typically involving materials like ferromagnetic stainless steel. These pose serious risks of either moving around inside the body or causing burns during scans and should never be exposed to MRI environments. Doctors need to check actual manufacturer labels that meet ASTM F2503 requirements rather than making assumptions based solely on materials. This approach ensures patients stay safe before they even step into the scanner room.
Why Anterior Cervical Anatomy and Implant Placement Amplify MRI Risks
The front part of the neck has an anatomy that makes MRI scans riskier than other body areas. Implants placed there are right next to important structures like the windpipe, food pipe, and major blood vessels that run through the neck. These structures can get affected by the strong magnetic fields during scans, either through physical forces or heat buildup. A small shift in position or even a slight temperature change might block someone's airway or damage blood vessels. Metal implants also create imaging problems because they mess with the MRI signals, making it hard to see critical areas such as the spinal cord, nerves, and where blood vessels branch off from the spine. These areas are essential when doctors need to check for conditions like spinal cord compression or narrowed spaces between vertebrae. The ASTM F2503 standard was developed specifically to handle these challenges. It tests how safe devices actually are in real world situations by recreating the worst possible placements against different tissues. This helps ensure that devices labeled as MR Conditional won't cause dangerous twisting, bending, or overheating issues in patients undergoing cervical spine imaging.
Material-Specific MRI Compatibility of Anterior Cervical Implants
PEEK Interbody Cages: Low Artifact Burden with Trade-offs in Structural Clarity
PEEK interbody cages made from polyether ether ketone material are considered safe for MRI scans because they don't contain metal or ferromagnetic components. These cages create very few image artifacts during both standard 1.5T and high strength 3T MRI scans. For doctors checking how well spinal fusions are working, looking at soft tissue issues, or spotting problems at nearby levels, this property is really helpful. The downside though? PEEK doesn't show up well on regular X-rays or CT scans, which can sometimes slow down diagnosis of cage or failed unions. The material's stiffness is around 3 to 4 GPa, which is actually softer than cortical bone. Some newer versions have been strengthened to handle loads closer to what happens naturally in the body. Doctors have seen good results with PEEK over time, especially in neck surgeries, when clear MRI images matter more than getting real time guidance during surgery itself.
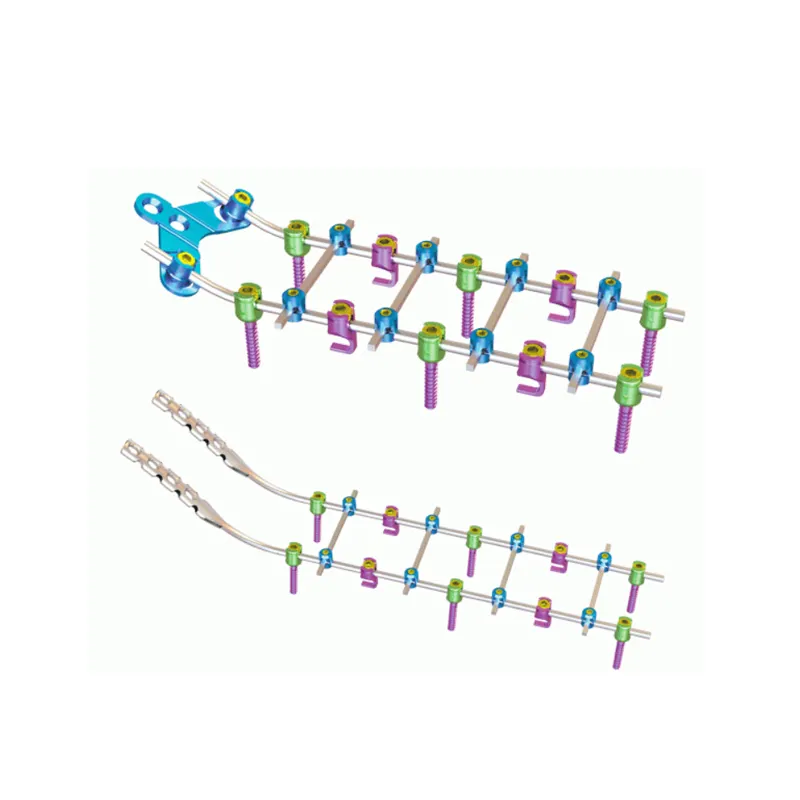
Titanium Alloys (Ti-6Al-4V, Ti-6Al-7Nb): Strength, Artifact Management, and Conditional Labeling Realities
For anterior cervical discectomy and fusion procedures, titanium alloys have long been considered the best choice for structural support due to their impressive strength relative to weight and their ability to integrate with bone tissue. However, these implants come with limitations when it comes to MRI compatibility according to ASTM F2503 standards. Surgeons need to be very careful about magnetic field strengths, gradients, and radiofrequency power levels during imaging. Although titanium creates fewer image artifacts than alternatives like stainless steel or cobalt chrome, there's still enough magnetic susceptibility to cause problems. We often see signal voids and distorted images around sensitive areas such as the spinal cord and blood vessels supplying the vertebrae. Research published in Acta Biomaterialia back in 2020 showed that porous titanium designs can cut down on these imaging issues by roughly 40% compared to traditional solid implants. Even so, radiologists working with patients who have these devices typically need to adjust their scanning techniques significantly. Techniques like tilting the viewing angle, preferring spin echo sequences instead of gradient echo, and increasing bandwidth settings help maintain image quality when examining those crucial neurological structures nearby.
Carbon Fiber Reinforced Polymer (CFRP) Cages: Emerging Standard for Artifact-Free Anterior Cervical MRI
Carbon fiber reinforced polymer cages bring together good mechanical strength with excellent imaging quality. CFRP materials are considered safe for MRI scans since they aren't magnetic, don't conduct electricity, and stay stable under heat changes. This means doctors get almost no image distortions even when using high field strength machines like 3 Tesla scanners. Research shows these cages create about 95-98% fewer image artifacts than titanium alternatives during standard 1.5T scans. That clear picture helps surgeons see important structures like the spinal cord, the protective covering around it, and nearby discs without obstruction. Better visibility makes it easier to spot problems such as nerve compression, fluid leaks, or recurring narrowing issues that need fixing again later on. While CFRP does come with a price tag roughly 30% higher than PEEK implants, many medical professionals find the improved diagnostic capabilities worth the extra expense, especially when dealing with complicated surgeries or patients needing multiple operations where accurate imaging matters most.
Integrating MRI Compatibility into Clinical Decision-Making and Workflow
Pre-MRI Screening: Leveraging Implant ID, Material Data, and Manufacturer Safety Documentation
For anyone with anterior cervical implants, thorough pre-MRI screening simply cannot be skipped. Standard metal detection isn't enough anymore. Clinicians need to check specific details about each implant according to ASTM F2503 standards. This includes looking at what materials were used and understanding those special conditions related to magnetic fields. Important factors are things like how strong the magnetic field can be, gradients across space, and safe absorption rates for radiation. A recent study by Ponemon Institute back in 2023 found something alarming: around seven out of ten MRI accidents with spinal implants happened because doctors didn't have all the right information about the implants. Good screening means making sure we know these specifics before proceeding with any scans.
- Torque and deflection limits for metallic plates or screws
- Whether PEEK or CFRP cages are labeled for artifact reduction
- Device-specific exclusions for high-field (3T+) or ultra-high-gradient scanners
Integrating implant databases directly into EHRs reduces screening errors by 32%, streamlining workflow while reinforcing patient safety.
Collaborative Protocols Between Surgeons, Radiologists, and Implant Representatives
Getting good results from MRIs while keeping patients safe really comes down to everyone working together ahead of time. When surgeons operate, they need to make sure they write down details about the implants used including what kind it was, the batch number, and whether it meets ASTM F2503 standards. This info needs to go into the medical records and get passed along to the radiology department well before any scan gets scheduled. The radiologists will look at these details and adjust how they run the MRI tests. They might choose a lower magnetic field strength like 1.5 Tesla when dealing with titanium implants, tweak timing settings, or use special techniques called MARS to reduce metal artifacts. Representatives from implant manufacturers often jump in during these discussions too, offering their expertise on what works best with specific devices. For example, they can suggest things like dynamic shimming for carbon fiber reinforced polymer implants or different contrast methods to check if PEEK cages have fused properly. Hospitals that implement this three-way collaboration between surgery, radiology, and manufacturer reps have seen some impressive improvements. One facility reported cutting down on unreadable cervical spine MRIs by almost half and reducing repeat scans significantly. Patients benefit from faster diagnosis and better outcomes overall.
Frequently Asked Questions
Are all anterior cervical spine implants safe for MRI scans?
No, not all cervical spine implants are automatically safe for MRI scans. Devices are categorized into MR Safe, MR Conditional, and MR Unsafe based on ASTM F2503 standards. It's crucial to consult manufacturer labels to understand the specific MRI conditions applicable.
Why is magnetic field strength important for MRI safety?
Magnetic field strength is critical because it determines how implants react to the MRI environment. MR Conditional implants have specific parameters such as field strength and gradient limits that need to be adhered to in order to ensure safety during the scan.
What makes PEEK cages favorable for MRI scans?
PEEK cages are favorable because they don’t contain metal or ferromagnetic components, resulting in fewer image artifacts during standard and high-strength MRI scans. However, they may have limitations when it comes to showing up on regular X-rays or CT scans.
 EN
EN
 FR
FR
 ES
ES
 AR
AR