Sterile Barrier Failures: The Leading Cause of Medical Device Packaging Recalls
Seal Integrity Breakdowns and Loss of Sterility in Implant Pouches
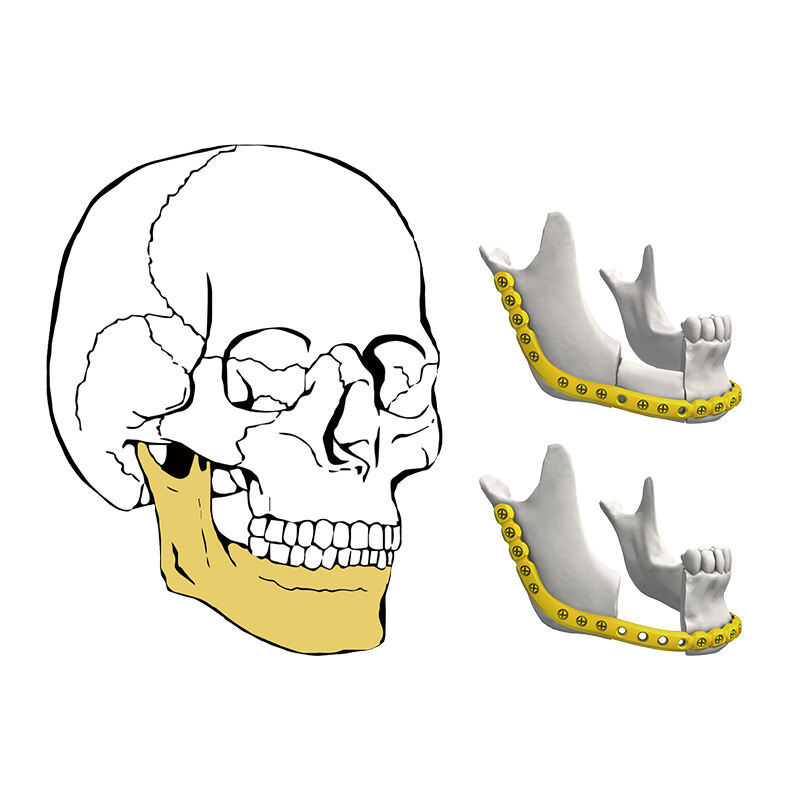
Sterile barrier systems act as the last line of defense against contamination for important medical devices such as mandibular reconstruction plates. Seal failures happen all too often through tiny channel leaks, adhesive coming loose from surfaces, or accidental punctures when staff handle the packages. Once this happens, microbes find their way in pretty much guaranteed. The connection between these failures and surgical site infections (SSIs) is pretty clear cut. The CDC reports around 1.7 million cases each year across hospitals nationwide. We see several common problems causing these issues: heat seals that aren't applied consistently during pouch production, materials breaking down after repeated exposure to changing temperatures, and particles getting trapped right where the seals meet. When these things occur, they completely undermine what ISO 11607 standards require for sterility, turning what should be protective packaging into something that actually spreads infection risks. With titanium implants that are sensitive to moisture, even small flaws in barriers speed up oxidation processes, which might change how well the implant integrates with surrounding bone tissue over time.
Case Study: 2022 FDA Recall of Titanium Mandibular Plates Due to Non-Intact Packaging
A 2022 FDA Class II recall led to the retrieval of 1,200+ titanium mandibular plates after visual inspections revealed packaging breaches. The investigation identified inadequate seal-width validation during accelerated aging tests and transport simulation protocols that failed to replicate real-world warehouse vibration stresses.
| Failure Factor | Clinical Consequence | Regulatory Gap |
|---|---|---|
| Pinhole leaks in sterile pouches | Bacterial colonization of implant surfaces | ASTM F2096 bubble testing not performed |
| Seal peeling under humidity | Loss of sterile field during OR presentation | Incomplete real-time aging data |
What happened really showed just how bad things got when ASTM F1980 took shortcuts with accelerated aging tests, especially since they relied so much on those perfect lab conditions. The problem is that real world situations throw all sorts of curveballs at products that aren't considered during testing. Things like sudden temperature changes while storing equipment or the rough treatment medical staff gives devices during emergency procedures simply weren't factored into the equation. After this big recall hit the news, companies across the board had to completely rethink their packaging strategies. Now manufacturers must check peel strength on each and every production batch, which adds time and cost but hopefully prevents similar issues down the road.
Inadequate Packaging Validation: Why ISO 11607 Compliance Falls Short
ISO 11607 sets out important guidelines for packaging validation, but just meeting these standards doesn't always stop problems in actual practice. Looking at what regulatory inspections find, roughly a third or so of issues with sterile barriers come from gaps in the validation process. These gaps tend to show up most frequently during accelerated aging tests and when simulating transportation conditions. The result? A lot of recalls happening for things like jaw reconstruction plates and other medical devices that literally save lives. Manufacturers need to look beyond basic compliance if they want to avoid these kinds of costly mistakes down the road.
Critical Gaps in Accelerated Aging and Transport Simulation Protocols
Most standard accelerated aging tests tend to miss those really harsh environmental factors that actually matter in practice. When it comes to transport simulations, they often forget about all sorts of shipping dangers we see in real life. Think about vibrations when switching between different modes of transport like air freight, or those unexpected temperature spikes in warehouses. What happens? Well, materials get fatigued faster than what labs predict. Take titanium mandibular plate pouches for instance. They might look great after passing lab tests, but surprise! Micro fractures start showing up once they hit the road for distribution. These gaps in testing mean sterile barriers can fail unexpectedly when faced with the messy reality of how products actually move through supply chains every day.
The Validation–Reality Disconnect: How Shelf-Life Testing Misses Clinical-Use Stressors
Most shelf life testing misses what actually happens when products get into real hands. Think about all those things that happen in practice: surgical trays knocking around packages, storage areas where items get squished together, fast sterilization processes that aren't gentle at all, plus people opening things wrong because they're rushed or impatient. Hospital staff sometimes place heavy instrument trays directly onto implant packages without thinking about it, or they pull open packaging so hard they break what was meant to protect contents inside. The accelerated aging tests only look at time and heat effects, completely overlooking the physical abuse packages receive while being moved between departments or opened in emergencies. That's why we see medical devices passing all their lab tests yet failing when used in actual surgeries. Packaging needs evaluation based on real world conditions, not just theoretical longevity standards.
Labeling Deficiencies and Human Factors Driving Medical Device Packaging Recalls
Ambiguous Sterilization Indicators and Confusing Expiration Logic
The problems with sterilization indicators start right at the basics. When they don't have clear visual signals or when their expiration dates don't fit how doctors actually work, this leads to a lot of packaging issues down the line. Take those color change strips for instance. If the colors aren't distinct enough or if it's hard to tell what counts as a pass versus fail, surgeons might get confused during operations where every second matters. According to some recent research, around one third of all recall incidents involving labels happen because medical staff simply read wrong information when rushed (the FDA did a survey on this back in 2021). Think about something specific like mandibular plates used in jaw surgery. If the label isn't clear, there's real risk that a doctor could end up using a device that wasn't properly sterilized, which puts patients in danger. These aren't just random packaging mistakes. They point to bigger problems in how medical equipment gets designed without considering actual users needs beyond meeting basic regulations.
The Growing Impact: Packaging-Related Recalls in Mandibular Implants (2019–2023)
Medical device packaging failures have become the biggest problem area for mandibular reconstruction plates according to recent FDA data. More than 60% of these issues involve broken sterile barriers. Looking at numbers between 2019 and 2023 shows something worrying too – recalls for these jaw plates went up by almost half compared to other orthopedic implants. Most problems happen when packages get damaged during shipping or while sitting on shelves. The current situation reveals some serious weaknesses in how well packaging holds up under actual distribution conditions instead of just passing lab tests. Mandibular plates present special challenges that other implants don't face. Their sharp edges and complicated shapes make packaging more prone to wear and tear, leading to punctures and leaks. When companies fail to properly test their materials and validation processes, what starts as random packaging flaws turns into widespread compliance problems throughout the industry. Manufacturers need to rethink their sterile barrier designs and start testing packaging in realistic distribution scenarios if they want to stop this growing issue before it causes harm to patients.
Frequently Asked Questions (FAQs)
What is a sterile barrier system?
A sterile barrier system is a protective packaging system designed to prevent contamination and maintain the sterility of medical devices until they are used.
Why are seal integrity and sterile barriers important for medical devices?
Seal integrity and sterile barriers are crucial because they prevent contamination by microorganisms, reducing the risk of infections during surgery or other medical procedures.
What are common causes of sterile barrier failures?
Common causes include channel leaks, adhesive failures, accidental punctures, and inadequate seal-width validation processes.
How can adherence to ISO 11607 standards impact medical device safety?
Adherence to ISO 11607 standards is important as these standards outline requirements for designing and validating packaging systems to ensure the sterility of medical devices.
What is the role of accelerated aging tests in packaging validation?
Accelerated aging tests simulate the effect of time on packaging materials to predict their longevity and ensure they continue to protect medical devices effectively over their intended shelf life.
Table of Contents
- Sterile Barrier Failures: The Leading Cause of Medical Device Packaging Recalls
- Inadequate Packaging Validation: Why ISO 11607 Compliance Falls Short
- Labeling Deficiencies and Human Factors Driving Medical Device Packaging Recalls
-
The Growing Impact: Packaging-Related Recalls in Mandibular Implants (2019–2023)
- Frequently Asked Questions (FAQs)
- What is a sterile barrier system?
- Why are seal integrity and sterile barriers important for medical devices?
- What are common causes of sterile barrier failures?
- How can adherence to ISO 11607 standards impact medical device safety?
- What is the role of accelerated aging tests in packaging validation?
 EN
EN
 FR
FR
 ES
ES
 AR
AR