Regulatory Foundations: EU GMP Annex 1 and ISO 14644 Alignment
EU GMP Annex 1 requirements for aseptic processing of sterile orthopedic implants
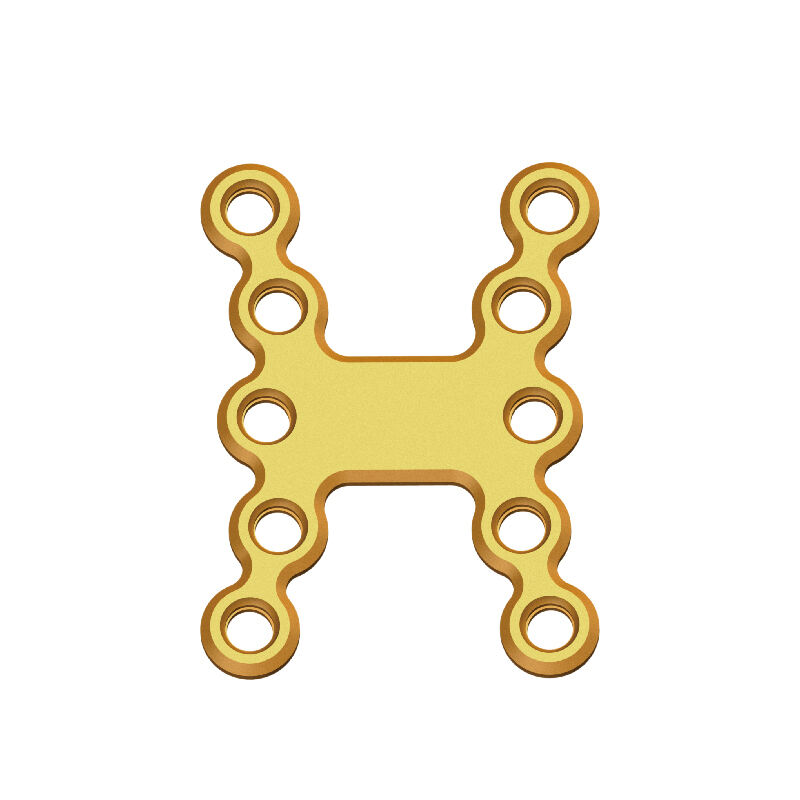
The EU GMP Annex 1 sets out pretty strict rules when it comes to keeping things sterile during the production of orthopedic implants like those sternum plates. Companies need to put in place sterilization methods that have been properly validated, keep tabs on their cleanrooms at all times, and make sure staff follow the right clothing procedures. When talking numbers, manufacturers have to show they can achieve a sterility assurance level no worse than 10^-6, which basically means there's less than a tenth of one percent chance something might not be sterile. How do they prove this? Through those media fill tests and proper validation processes. Some key stuff they need to control includes having that special filtered air moving in one direction in the top grade cleanrooms (Grade A or ISO Class 5), watching particles in real time while putting products together aseptically, and doing regular sterility checks according to standards laid out in ISO 11737-2.
ISO 14644-1 classification and monitoring expectations for Class 5 and Class 7 cleanrooms
The ISO 14644-1 standard puts cleanrooms into different categories depending on how many particles float around in the air. For instance, Class 5 spaces are typically where they handle things like sterile plate manufacturing, and these rooms can't have more than about 3,500 particles per cubic meter when looking at particles 0.5 microns or larger. Then there's Class 7 environments which are generally for support activities rather than core production work. These allow significantly more particles - around 350 thousand per cubic meter using the same measurement criteria. Interestingly enough, this system matches up pretty well with what's outlined in the EU GMP Annex 1 guidelines too. Grade A cleanrooms basically map to our ISO Class 5 standards while Grade B falls right into line with Class 7 specifications according to those regulations.
| Parameter | Class 5 | Class 7 |
|---|---|---|
| Particle count (≥0.5μm) | ≤3,520/m³ | ≤352,000/m³ |
| Air changes/hour | ≥240 | ≥60 |
| Pressure differential | +10–15 Pa | +5–10 Pa |
Cleanrooms require recertification every 6–12 months, with documented risk assessments guiding sampling locations and frequencies to ensure sustained compliance.
Core Monitoring Modalities: Viable and Non-Viable Particle Control
Active air sampling and settle plates for microbial environmental monitoring cleanroom sternal plates
When it comes to keeping track of living microbes floating around in cleanrooms where sternal plates get made, there are basically two main approaches: active air sampling and settle plates. These work together pretty well actually. With active sampling, special equipment pulls air through growth media so we can count exactly how many colony forming units (CFUs) are present at different points during manufacturing. This gives us hard numbers about what's happening in the air when things matter most. Then there are those settle plates sitting out for around four hours collecting whatever falls down from above. They act like little traps showing us what might land on sensitive areas like open implants if something goes wrong. Both methods tell different parts of the story about potential contamination risks in these controlled environments.
The ISO 14644-1 standard actually specifies maximum allowable colony forming units per cubic meter at different cleanroom classifications. For instance, Class 5 areas must stay under 1 CFU/m³ while Class 7 spaces can tolerate up to 10 CFU/m³. Putting monitoring equipment strategically close to where sterile operations happen makes it possible to catch problems before they become major issues. Settle plates are great for spotting contamination sources related to people moving around or when materials get transferred between zones. But don't forget about active air sampling which does a much better job revealing if the heating, ventilation and air conditioning system is performing properly. These two methods working together create what many facilities consider their best defense against microbial threats, helping ensure products remain free from contamination during critical manufacturing steps.
Laser particle counter protocols for real-time non-viable particulate monitoring
Laser particle counters are really useful for keeping track of those tiny non-living particles down at 0.5 microns and above, all the way up to 5 microns too. This kind of monitoring is super important if we want to stay within ISO Class 5 standards. We usually put these sensors in spots where contamination risks are highest, think about areas around filling stations or where products get packaged. When the count goes past that magic number of 3,520 particles per cubic meter, the system lets everyone know right away. If there are multiple readings outside the normal range, automated systems kick into action, prompting staff to look into what might be going wrong. Corrective measures can then be taken quickly, whether it means adjusting airflows or temporarily stopping operations until things get back under control.
The ability to maintain clean conditions becomes really important when packing sternal plates because even tiny particles getting inside can mess up the sterile environment needed for surgery. When looking at medical device regulations, proper documentation plays a big role. According to recent reports from last year, almost all FDA warning letters mentioned problems related to tracking these particles somewhere in their findings. During procedures considered risky for contamination, teams tend to check things more often. This makes sense since they need to stay on top of potential issues while maintaining good control over the environment throughout the whole process.
Surface and Personnel Monitoring: Critical Controls for Sterility Assurance
Contact plates, swabs, and glove print testing for sternal plate production zones
Surface and personnel monitoring serve as the final barrier against contamination in sterile sternal plate manufacturing. Contact plates are used to sample flat, accessible surfaces in ISO-classified zones, detecting viable microorganisms post-processing. For complex or recessed equipment geometries, pre-moistened sterile swabs provide targeted sampling where contact plates are ineffective.
Monitoring staff involves collecting glove prints right after they perform sterile procedures, plus taking samples from their gown sleeves when shifts wrap up. Frequent testing becomes really important during those parts of production where people have to handle things manually, since this is when there's a higher chance of getting contaminants into the product. Looking at data from 2023 on sterility failures shows something pretty alarming: nearly seven out of ten problems with orthopedic implants came from either gloves or surfaces being dirty. All these different checks work together to help reach the necessary standards for sterility, which makes them a core part of keeping aseptic processes clean and effective throughout manufacturing.
Risk-Based Monitoring Strategy: Frequency, Location, and Documentation
Sampling point rationale: airflow mapping, critical process steps, and personnel movement
Good environmental monitoring starts with picking the right spots for samples based on actual science. When we map out airflow patterns, we can spot those tricky areas where dust and particles tend to hang around near sensitive parts. That helps us know exactly where to put our sensors and collection plates. The real action happens during key manufacturing stages like when moving implants between stations, putting them together, and wrapping them up for shipment. These are the moments when things can go wrong with sterility. We also keep a close eye on areas where staff move frequently because people walking around is actually responsible for about 70 to 80 percent of all contamination problems in cleanrooms. By focusing on these three main risk areas, manufacturers get full coverage against the biggest threats to product quality in their sterile implant production lines.
Defining monitoring frequency per zone and linking to contamination risk assessment
Monitoring frequency is determined by cleanroom classification and risk level, ensuring proportionate oversight. Class 5 zones, where sternal plates are exposed, require continuous non-viable particle monitoring and daily microbial sampling. Class 7 support areas typically undergo weekly microbial checks, with frequency adjusted based on historical data and risk assessments.
This tiered strategy optimizes resource use while maintaining compliance with ISO 14644 and EU GMP Annex 1. Review and adjustment of monitoring plans occur quarterly or following process changes, ensuring ongoing alignment with contamination control objectives and regulatory expectations.
FAQ
What is the main purpose of EU GMP Annex 1?
The EU GMP Annex 1 provides stringent guidelines to ensure the sterility of pharmaceutical products and medical devices during manufacturing, requiring validated sterilization processes and cleanroom maintenance.
How does ISO 14644 classify cleanrooms?
ISO 14644 classifies cleanrooms based on the concentration of airborne particles, with classes ranging from 1 (very clean) to 9 (less clean), ensuring controlled environments for different applications.
Why are settle plates and active air sampling used together?
Both methods assess microbial contamination in cleanrooms; settle plates gauge particulates that fall onto surfaces, while active air sampling measures airborne CFUs during crucial manufacturing steps.
How often should cleanrooms be recertified?
Cleanrooms require recertification every 6–12 months to ensure material conditions remain compliant with set standards.
What risks do laser particle counters mitigate?
Laser particle counters detect non-viable particulates in real-time to prevent contamination during sensitive manufacturing processes, alerting staff to deviations so corrective measures can be applied promptly.
 EN
EN
 FR
FR
 ES
ES
 AR
AR