Why Titanium Mesh Composite Demands Specialized Sterilization Methods
Key material properties affecting sterilization compatibility
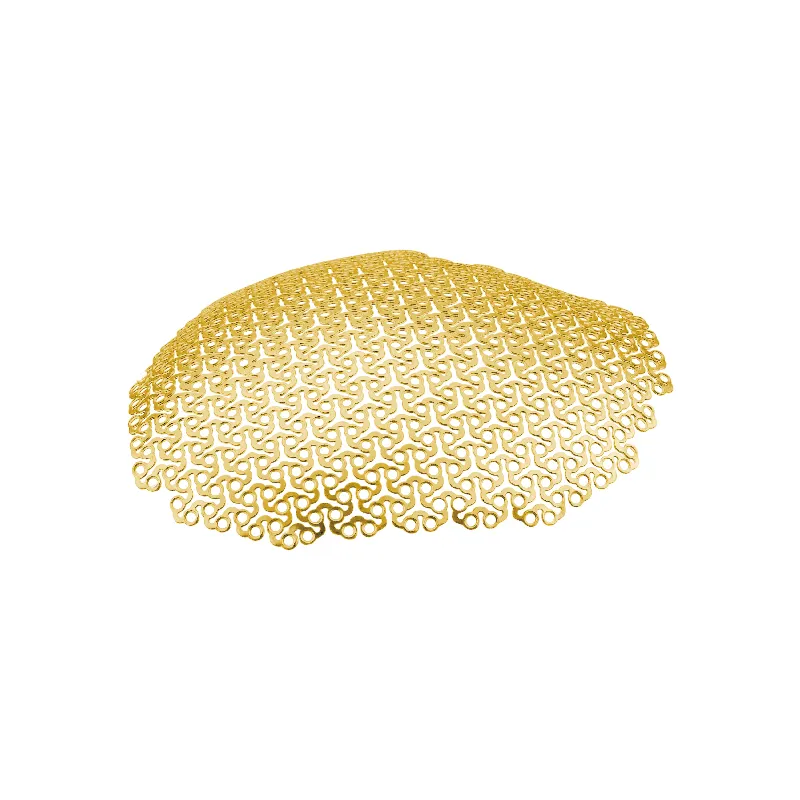
The porous structure and mixed makeup of titanium mesh composites present some real problems when it comes to sterilization. These materials combine metal titanium with either polymers or ceramics, which creates issues during cleaning processes. The large surface area along with all those tiny spaces between the material particles tends to hold onto biological contaminants and leftover substances. Plus, certain parts of these composites are sensitive to heat or radiation and tend to break down when exposed to standard sterilization techniques. Gamma radiation works well with titanium itself but causes problems for the polymer parts, cutting their tensile strength by about 15 to 30 percent after multiple exposures. Steam sterilization at temperatures over 121 degrees Celsius leads to layer separation in around 40 percent of test samples. All these issues highlight why we need better control over specific sterilization parameters. It's not enough just to kill microbes; maintaining the physical structure and functionality of these composite materials is equally important.
Biocompatibility, corrosion resistance, and structural stability under sterilization stress
Sterilization directly influences clinical performance across three interdependent domains:
- Biocompatibility preservation: Residual ethylene oxide (EtO) adsorbs onto porous surfaces, triggering inflammatory responses in ~12% of implant cases—highlighting the risk of chemical carryover in low-temperature methods.
- Corrosion resistance: Autoclaving cycles accelerate breakdown of titanium’s protective oxide layer, tripling corrosion rates in saline environments and raising concerns about long-term implant degradation.
- Structural integrity: Thermal stress from steam sterilization generates micro-fractures at titanium-polymer interfaces, reducing fatigue resistance by up to 25%.
Validated protocols must therefore maintain surface chemistry and interfacial cohesion. Low-temperature alternatives like vaporized hydrogen peroxide (VHP®) avoid thermal damage and leave no toxic residues—but require material-specific validation to confirm absence of residual peroxides that could impair biocompatibility or trigger oxidative stress in vivo.
Proven Sterilization Methods for Titanium Mesh Composite
Gamma radiation: Gold standard for terminal sterilization of titanium mesh composite
Gamma radiation is still considered the gold standard when it comes to killing germs on those titanium mesh composite implants that need sterilizing before surgery. What makes this method so reliable? Well, those powerful gamma rays can get through sealed packages evenly, hitting that super important sterility assurance level of 10^-6 as set by ISO 11137 standards. Plus, there's no mess left behind from chemicals or heat damage. Medical facilities typically use doses between 25 to 40 kilograys because these levels have been tested extensively to keep the titanium from corroding, maintain its strength under pressure, and ensure it plays nicely with human tissue over time. This matters a lot for implants that need to hold weight or stay in place for years. Another big plus is how well gamma radiation works with complicated shapes and allows sterilization right in the final packaging. That means manufacturers can streamline their production lines for Class III medical devices without extra steps. Compared to other methods like heat treatment or gas fumigation, gamma doesn't leave behind any nasty smells or require waiting periods after processing. Makes sense why hospitals and manufacturers prefer it for urgent cases or when they need to produce large quantities quickly.
Steam sterilization (autoclaving): Limits, thresholds, and validated use cases
Steam sterilization works for titanium mesh composites but only when everything is just right, and mostly for things that won't go inside people or get used once and thrown away. The standard autoclave settings (around 121 degrees Celsius, 15 pounds per square inch pressure, lasting 15 to 20 minutes) can actually cause problems over time. After about five cycles, there tends to be more separation at the interfaces in these polymer reinforced materials. Pure titanium parts can handle brief exposure to temperatures as high as 135°C according to some approved methods, though nobody should skip doing those accelerated aging tests first to figure out exactly how many cycles each specific device can take. Surgical guides and other temporary equipment do well with autoclaving because it's fast and easy to access, as long as we don't leave them in the steam for longer than 30 minutes at a stretch. Still, nobody really recommends using autoclaves for the final sterilization step on implantable composites unless they've done all sorts of testing specific to that particular material type. The heat is just too harsh and doesn't penetrate properly into those dense areas with lots of pores.
Low-Temperature Sterilization Options for Heat-Sensitive Assemblies
Vaporized hydrogen peroxide (VHP®) compatibility with titanium mesh composite
Vaporized hydrogen peroxide (VHP®) works as a tested option for sterilizing titanium mesh composites when traditional methods like gamma radiation or steam aren't feasible because of heat issues or packaging limitations. The process runs between 40 to 50 degrees Celsius and kills microbes effectively through reactive oxygen species without damaging the protective oxide layer on titanium or compromising the polymer parts. Research published in reputable journals shows that VHP gets into those tricky porous areas without causing corrosion problems or leaving behind harmful residues that could affect cells. How long it takes depends on what's being sterilized inside the chamber, usually taking anywhere from half an hour up to almost an hour and fifteen minutes for more complicated setups. What makes VHP really useful is that it plays nicely with regular medical packaging materials too. For anyone needing to choose a sterilization method for these titanium mesh products, VHP offers a good mix of meeting regulations, keeping materials intact, and working well with already packaged items ready for use.
Ozone and other emerging low-temperature alternatives: Evidence and gaps
Ozone sterilization has some theory behind it - things like working at room temperature, fast processing times, and being better for the environment - but there's still not enough proof when applied to titanium mesh composites. Early tests do show pathogens getting killed off through oxidation processes, though several issues hang over this approach. What happens to titanium surfaces over time? Does the protective oxide layer wear down? How well does it work with different polymers? Nitrogen dioxide plasma looks promising too for quick processing without leaving residues, but nobody has worked out proper validation standards for titanium implants through ISO or FDA channels yet. We're missing key information about how good these methods really are against stubborn biofilms, what happens to materials after repeated sterilizations, and managing any leftover substances, especially in those complicated multi-layer structures. Until someone publishes solid research showing these techniques work safely and reliably in all sorts of medical situations, they'll stay as backup options rather than going mainstream.
Selecting the Optimal Sterilization Method for Clinical and Regulatory Success
Choosing the right sterilization approach for titanium mesh composites requires balancing what doctors need, how materials behave, and what regulations demand. According to recent FDA guidelines from 2023 plus standards set by ISO 13485:2016, companies have to test every sterilization process with biological indicators. They also need to show that their Sterility Assurance Level meets or exceeds 10^-6 for medical implants. Along with these basic requirements, there's plenty more to consider too. Manufacturers should thoroughly check if the material stays stable after treatment, monitor any changes in surface chemistry, and ensure all functional properties remain intact. When it comes down to making decisions about sterilization methods, three main considerations tend to stand out above everything else:
- Material compatibility: Gamma radiation requires confirmation that doses do not induce titanium embrittlement or polymer chain scission; VHP® demands verification of peroxide decomposition kinetics to rule out residual cytotoxicity.
- Device geometry and porosity: Complex, high-surface-area constructs favor penetrating modalities like gamma or VHP® over diffusion-limited gases or steam.
- Production scale and lifecycle needs: High-volume implant manufacturing favors gamma’s scalability and consistency; lower-volume or custom devices may justify VHP®’s flexibility and reduced infrastructure investment.
Getting regulatory approval isn't just about picking the right method. What really matters is showing consistent control over key factors like dose levels, concentrations, temperatures, and how long things are exposed. There also needs to be clear documentation proving sterility has been achieved without messing up corrosion resistance, structural strength, or causing unwanted reactions from the body. Good validation strategies typically include accelerated aging tests, surface analysis techniques such as XPS and SEM scans, plus laboratory testing for biocompatibility. These combined approaches help ensure medical devices work properly, stay safe, and perform reliably during their entire expected use in clinical settings.
FAQ
What challenges do titanium mesh composites face in sterilization?
The porous structure and mixed material makeup of titanium mesh composites can retain biological contaminants, and some components are sensitive to heat or radiation.
Why is gamma radiation a preferred method for sterilizing titanium mesh composites?
Gamma radiation effectively kills germs without leaving residues and maintains material integrity, even for complex shapes and high-volume manufacturing.
What are the disadvantages of using steam sterilization on titanium mesh composites?
Steam sterilization can cause layer separation and micro-fractures due to thermal stress, especially with repeated cycles.
How does vaporized hydrogen peroxide work as a sterilization method?
Vaporized hydrogen peroxide sterilizes effectively at low temperatures while protecting titanium's oxide layer and polymer components.
Table of Contents
- Why Titanium Mesh Composite Demands Specialized Sterilization Methods
- Proven Sterilization Methods for Titanium Mesh Composite
- Low-Temperature Sterilization Options for Heat-Sensitive Assemblies
- Selecting the Optimal Sterilization Method for Clinical and Regulatory Success
-
FAQ
- What challenges do titanium mesh composites face in sterilization?
- Why is gamma radiation a preferred method for sterilizing titanium mesh composites?
- What are the disadvantages of using steam sterilization on titanium mesh composites?
- How does vaporized hydrogen peroxide work as a sterilization method?
 EN
EN
 FR
FR
 ES
ES
 AR
AR