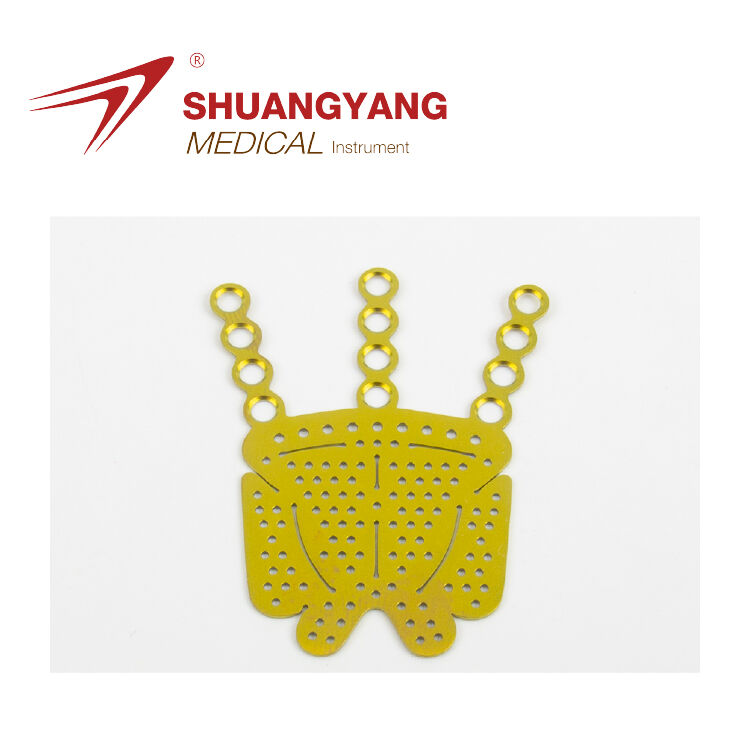
Definition of Tissue Compatibility in the Context of Orbital Biomaterials
When we talk about tissue compatibility, we're really looking at how well a material works inside the body without causing problems like immune reactions or toxicity. For those orbital plate implants specifically, finding the right balance between being strong enough structurally and not reacting chemically with surrounding tissues is key to avoiding rejection issues. Recent research from 2023 shows these implants have pretty good long term results too, with over 95% success rate when there aren't any inflammatory complications. But compatibility isn't just about staying put without trouble. Good materials actually help new tissue grow properly around them. This matters a lot in the delicate bones around the eye area where even small stresses can lead to fractures or other problems down the road because the bone structure is so thin and fragile there.
Role of Biological Materials and Tissue Compatibility in Implant Success
What really matters for good clinical results comes down to three main factors. First, materials need to stay stable when exposed to body fluids. Second, surfaces should have tiny pores (around 60 to 70 percent seems best) that help bones grow around them. Third, they must resist breaking down so ions don't leak out into surrounding tissues. New composite materials are making progress here, degrading at about half a millimeter per year which matches what we see with titanium implants but creates much clearer images during scans. Recent improvements in how surfaces are treated mean PEEK implants can now make contact with bone at levels similar to titanium, hitting about 92 percent effectiveness thanks to special bonding methods involving hydroxyapatite. This makes them work better with living tissue while keeping their strength intact.
Key Factors Influencing Histocompatibility of Implant Materials and Their Biocompatibility
| Factor | Impact Threshold | Clinical Relevance |
|---|---|---|
| Surface Roughness | Ra 1.5–4.5 µm | Optimizes fibroblast adhesion |
| Elastic Modulus | 10–25 GPa | Matches orbital bone biomechanics |
| Ion Release Rate | ≤0.05 µg/cm²/day | Prevents peri-implant osteolysis |
| Hydrophilicity | Contact angle <75° | Enhances protein adsorption efficiency |
Material selection increasingly favors multiphasic designs combining load-bearing cores like Ti-6Al-4V with bioactive surfaces such as porous tantalum or nitinol. When paired with antimicrobial coatings, these hybrid systems achieve a 98% five-year survival rate even in infected wound beds, underscoring their resilience and biocompatible performance.
ISO 10993 Standards for Orbital Implant Biocompatibility Testing
Overview of ISO 10993 Compliance Requirements for Orbital Plates
For orbital plates used in medical applications, compliance with ISO 10993 is absolutely necessary since this is the worldwide standard for ensuring biocompatibility in medical devices. The standard requires thorough testing protocols to make sure these implants won't cause harmful reactions inside the body. Testing typically covers several key areas including cytotoxic effects according to ISO 10993-5, potential skin sensitization per ISO 10993-10, possible irritation responses, and systemic toxicity as outlined in ISO 10993-11. These tests are crucial because they help confirm that the materials remain safe even when in long term contact with the sensitive tissues around the eye socket area.
Cytotoxicity, Sensitization, and Irritation Testing: Core Safety Evaluations for Orbital Plate Tissue Compatibility
Testing for cytotoxicity helps find materials that damage cells, which is really important since implants often sit close to sensitive eye tissues. Then there are tests for sensitization that check if something might cause allergies, and separate tests look at whether materials trigger local inflammation when they come into contact with body tissues. Take polymer plates as an example. These go through multiple rounds of exposure testing that mimic what happens over about 30 days of actual tissue contact. The whole process follows guidelines from ISO 10993-10 standards, making sure these materials stay compatible with living tissues over time rather than just passing initial checks.
Systemic Toxicity and Implantation Testing Under ISO Guidelines
The ISO 10993-11 standard looks at systemic toxicity through extract analysis methods that help identify how leachable substances might affect different organs in the body. According to ISO 10993-6 guidelines, researchers must also implant materials into animal models for a minimum of twelve weeks to observe what happens with local tissues over time. When it comes to titanium alloys, they tend to perform quite well in these tests. Studies show these alloys result in under 5% fibrotic encapsulation when used around eye areas, which makes them significantly better than stainless steel options. The difference is about 20% improvement according to histocompatibility measurements, making titanium a preferred choice for many biomedical applications where long term compatibility matters most.
Biological Responses to Orbital Biomaterials Over Time
Immune Response and Foreign Body Reaction to Non-Resorbable Orbital Plates
Orbital plates that don't get absorbed by the body are usually made of titanium or special medical plastics, and they tend to cause what doctors call a two stage immune reaction. About four to six weeks after implantation, the body sends out these cells called macrophages along with fibroblasts to the area where the plate is placed. These cells form this sort of fibrous wall around the implant, basically creating a barrier between the foreign object and surrounding tissues. According to research published by the Biomaterials Society last year, this happens in roughly two thirds of all cases with non resorbable implants. On one hand, this capsule helps reduce rubbing between the tissue and the metal plate. But there's another side to it too the capsule can actually leave tiny gaps where bacteria might start growing, which could eventually affect how stable the implant remains over time.
Tissue Integration and Degradation Profiles of Bioresorbable Implants
Materials that can be absorbed by the body like poly-L-lactic acid (PLLA) work quite differently when they come into contact with surrounding tissues. The implants slowly break down over time, allowing about 94 percent of new tissue growth around them within roughly six months to maybe even a year or so. This gradual breakdown actually matches pretty well how bones naturally change shape during healing processes. But there's a problem if these materials start dissolving too quickly before reaching that six month mark. When this happens, patients face a 22% higher chance of experiencing orbital floor collapse issues. That's why engineers really need to get creative with their designs, matching each implant specifically to how fast different people heal from surgery.
Inflammatory Response Dynamics and Long-Term Biocompatibility Monitoring
Getting good biocompatibility really depends on getting rid of that initial inflammation within about three months after surgery. If neutrophils keep hanging around past that 90 day mark, studies show people face almost four times the chance of developing chronic pain or having their implanted devices move out of place according to Clinical Implant Review from last year. Doctors are now using something called contrast enhanced MRI along with checking blood levels of IL-6 to catch these problems before they become serious. This approach has worked pretty well too, catching issues early in nearly nine out of ten patients who were considered at high risk for complications.
Comparative Biocompatibility of Orbital Plate Materials
Metal vs. Polymer vs. Composite: Material Performance in Tissue Compatibility Testing
Titanium alloys are known for their impressive mechanical strength, typically ranging from around 380 to 460 MPa in yield strength. However, these materials sometimes cause problems too, with studies indicating that about 12 to 18 percent of patients experience some kind of foreign body reaction according to research published by Tang and colleagues back in 2020. Looking at polymers instead, materials such as PCL and PLA tend to integrate well with tissues initially. The downside? These polymers break down significantly quicker than composite materials when placed in real physiological conditions, degrading approximately 30 to even 45 percent faster over time. Hybrid approaches have emerged as promising alternatives though. Take hydroxyapatite reinforced polymers for instance. These combine good osteoconductive qualities with pores making up roughly 85 to 92 percent of their structure. What's really interesting is how they allow for adjustable resorption rates. Early tests actually showed these hybrids promote about 15 percent more bone growth compared to traditional metal implants in preliminary animal studies.
| Material Class | Advantages | Limitations |
|---|---|---|
| Metals | High load-bearing capacity, sterilization stability | Potential for imaging artifacts, stress shielding |
| Polymers | Customizable degradation, MRI compatibility | Limited long-term mechanical strength |
| Composites | Balanced bioactivity and durability, 3D-printable | Complex manufacturing requirements |
Clinical Outcomes of Resorbable Versus Non-Resorbable Implants in Orbital Reconstruction
The PLLA/PLGA resorbable implants manage around 94% tissue integration after about six to nine months, which sounds pretty good on paper. However, these materials need extra support in roughly one out of every five trauma situations because they tend to weaken structurally too soon. On the other hand, non-resorbable titanium mesh keeps things anatomically accurate with deviations under 1.2 mm, making it very precise. But there's a catch: about 8 to 10 percent of patients experience chronic inflammation issues within five years. Recent research from multiple centers in 2023 showed that composite resorbable options cut down the need for repeat surgeries by almost half when compared against traditional permanent implants. That said, doctors should be aware that these newer composites come with about 18% more instances of swelling right after surgery than their counterparts.
FAQ Section
What is tissue compatibility in orbital implants?
Tissue compatibility refers to how well an implant material performs inside the body without inducing immune reactions or toxicity. Achieving this balance is crucial for avoiding implant rejection.
Why is ISO 10993 important for orbital plates?
ISO 10993 is the global standard for ensuring biocompatibility in medical devices. Compliance with this standard ensures that orbital plates do not cause harmful reactions within the body.
What are the advantages of titanium alloys in orbital implants?
Titanium alloys are preferred for their mechanical strength and low fibrotic encapsulation rates, making them a suitable choice for biomedical applications.
How do resorbable implants differ from non-resorbable ones?
Resorbable implants gradually break down over time, promoting tissue integration, whereas non-resorbable implants maintain their structure but might cause immune reactions.
Table of Contents
- Definition of Tissue Compatibility in the Context of Orbital Biomaterials
- Role of Biological Materials and Tissue Compatibility in Implant Success
- Key Factors Influencing Histocompatibility of Implant Materials and Their Biocompatibility
- ISO 10993 Standards for Orbital Implant Biocompatibility Testing
- Biological Responses to Orbital Biomaterials Over Time
- Comparative Biocompatibility of Orbital Plate Materials
- FAQ Section
 EN
EN
 FR
FR
 ES
ES
 AR
AR